It is now 12 years since I was diagnosed with having a neurological condition that results in a lot of brain damage and early-onset dementia. In my case it also resulted in the shaking and instability of Parkinson’s disease and what many would confuse with Alzheimer’s disease. In 2012, retired from 35 years of being a California-licensed research psychologist who had most recently worked evaluating more than 200 agencies that were affiliated with hospitals and community organizations and provided services to people were ignored in the larger health care system in the US. Together with my business partner Dr Lisa Melchior, our consulting worked with the patients-clients-staff-administrators programs funded through grants from Federal agencies in 42 states as well as State Departments of health, education, and research, and foundations, corporations, and individual donors.
When I was forced to retire because of my deteriorating health and my concerns that I would make a mistake and misinterpret data being collected in our research on innovative treatments for underserved and stigmatized people, I decided that I would spend my final years trying to develop some techniques assisting underserved people with dementia, their caregivers, and their medical providers to have the highest quality of life possible at their levels of physical and mental disease. As a side note, I cringed every time some well-meaning friend, colleague, or acquaintance suggested that I should develop a “bucket list” of all the places I never traveled to on vacations or in my work. Many thought the 6 million “miles” I had accumulated in my frequent flyer account meant I love to travel nonstop. Rather, 90 percent of the time, I preferred to be at home working on things important to me.
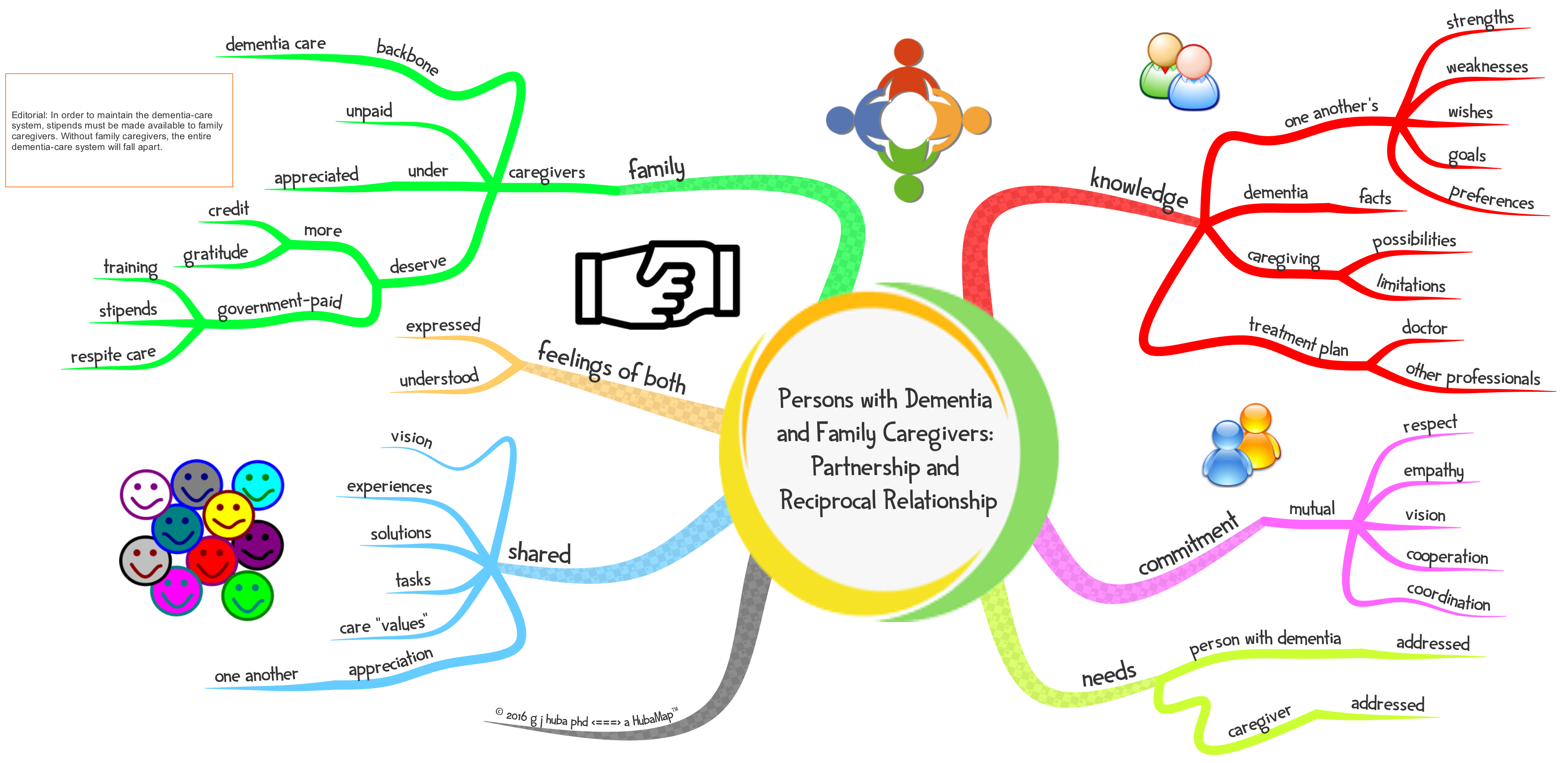
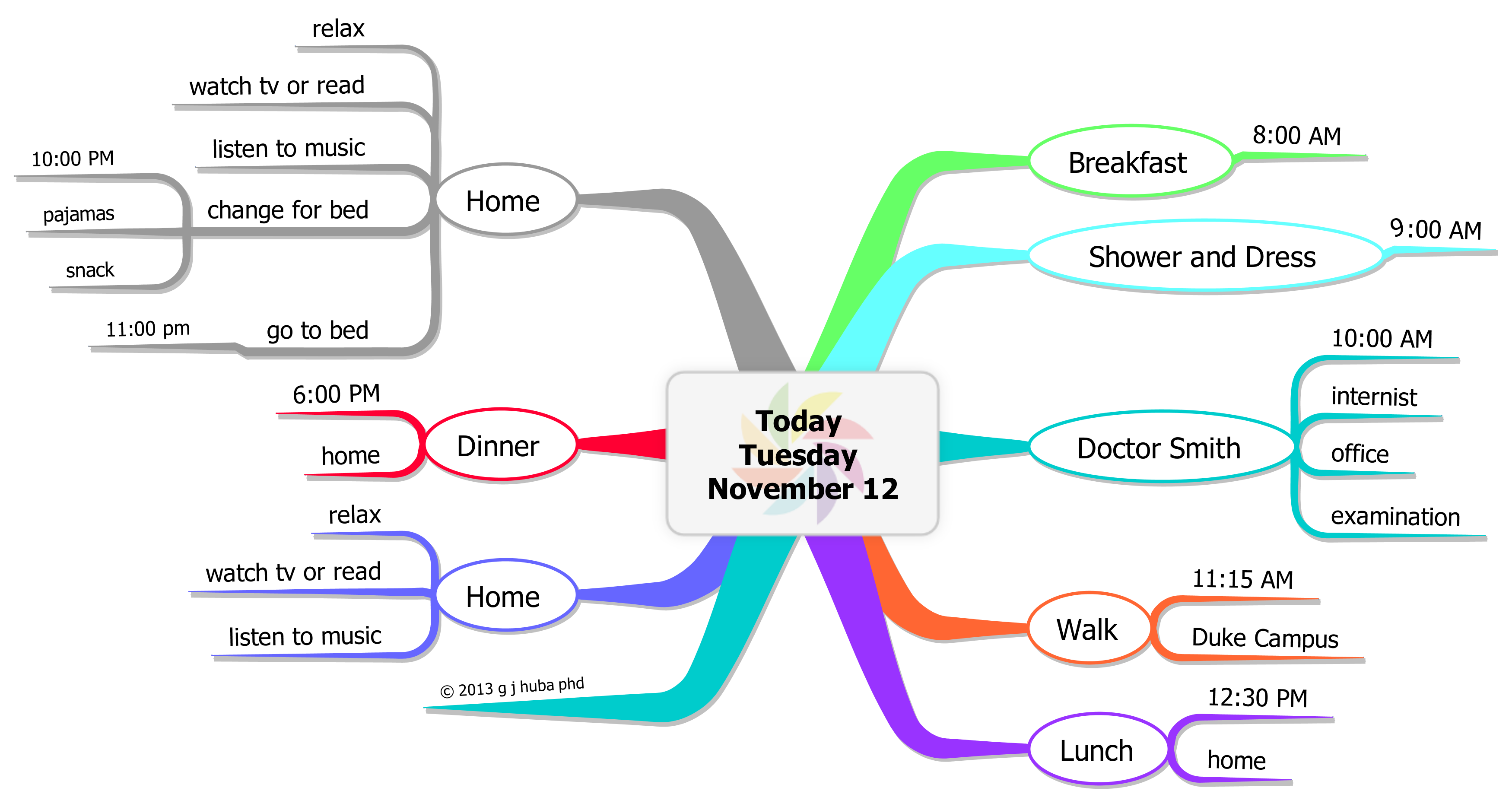
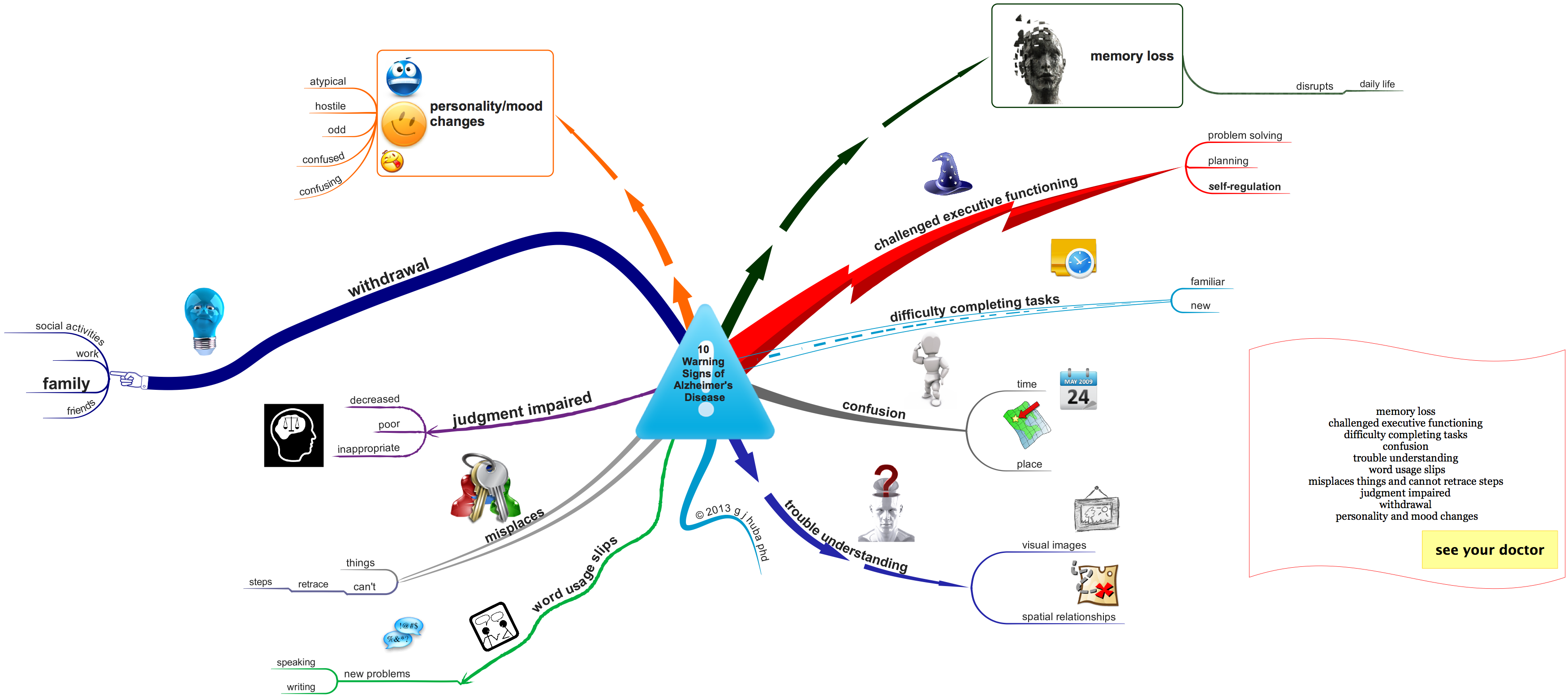
So I focused on developing inexpensive, easy-to-use methods one could use to find the good things in life and enjoy them, support family members and others in caregiving, and let doctors like myself see what it like to be living with dementia. My belief that is that those with dementia are capable of more than watching old TV shows all day, “abusing” their caregivers by because of frustration, and being “drugged” to a point where they lose focus and an ability to make themselves happy, productive, empathic, and content with their lives within a new reality that is confusing and frustrating. I think that some of the simple methods I have developed and expanded in the 999 blog posts before this one, can be used by many, far at times fun to do, do not require the help of others, and very inexpensive (you can do what I do with a pencil and the back of an used envelope.
I am now developing a second web site Huba.com that is much more direct in helping one to learn my techniques, determine if they are useful for them, and perhaps have an enhanced quality of life. Unlike this web site which more historical, scientific, and experimental, the new web site will be very focused on “just doing it” and enjoying the rest of your and not wrecking the lives of others.
I have done a lot of work which has been fun in the past 12 years. Work has also been my hobby my whole life, and most days at least most of the time I was happy.
Here is a summary of some of the major things that have been going on recently. And … the new web site will be fully operational within a few months.
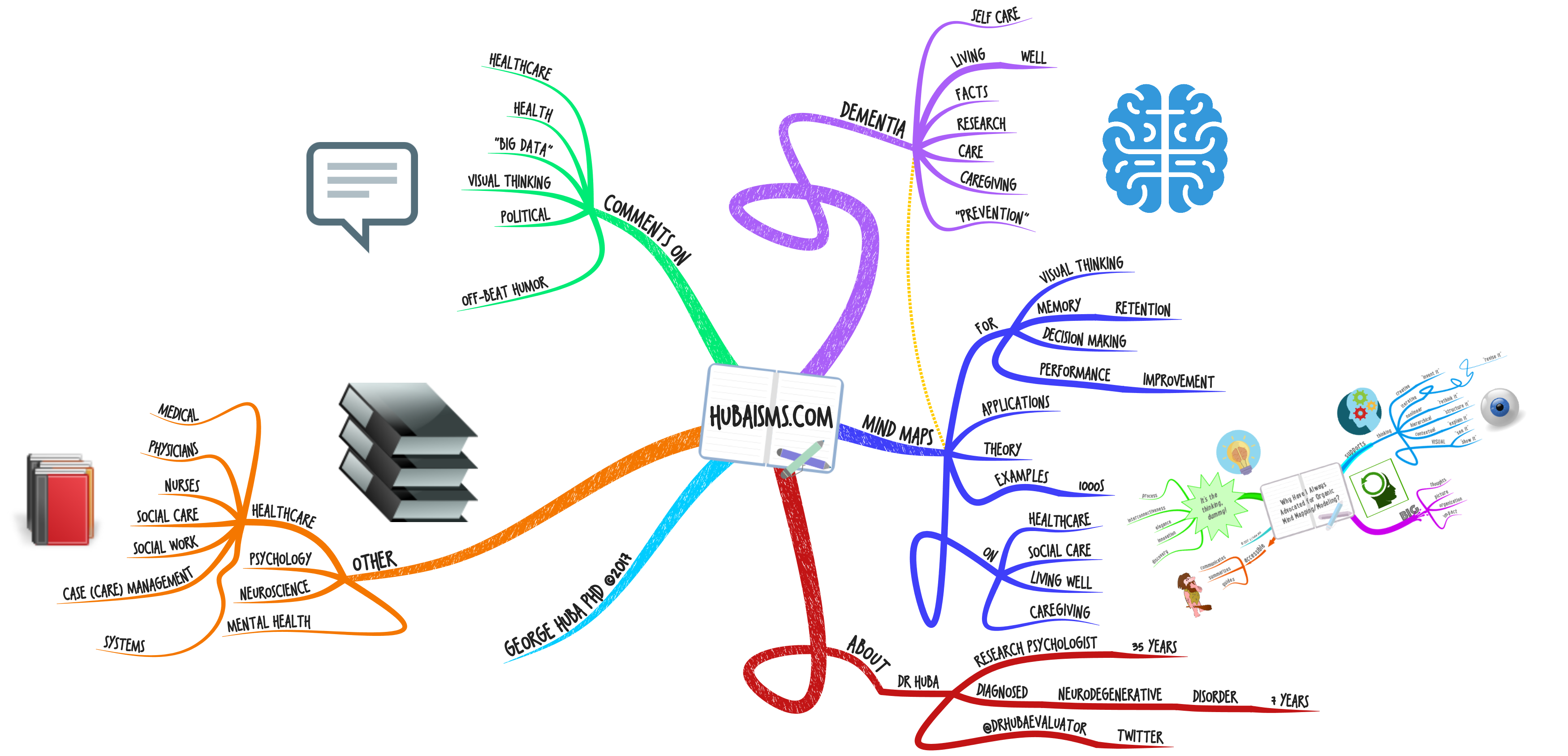
To make the following mind map larger, you can double-click on the picture and it will expand.
or