In March 2018, @USNews and @AetnaNews published key results from their study of approximately 3,000 US counties. Each of these counties received a total score as an index of how healthy the community is as well as scores on 10 component parts of being a healthy community. Eighty indicators of community health were developed from standard, well-constructed, and valid datasets.
The Healthiest Communities rankings are based on well-collected longitudinal survey data from US government databases and those of well-established, not-for-profit organizations.
Click here to see the full report in a new window.
My professional conclusion is that the study is valid, reliable, and relevant. The index scores are based on a combination of expert judgment from independent professionals and data sources that are among the best available. Statistical analyses appear to be appropriate and expertly applied. Of course, as with all such studies, over time additional analyses can be made, interpretations can be added by experts of many disciplines not limited to health, and supplemental quantitative (numerical) and qualitative (judgment) data can be collected.
The report on America’s Healthiest Communities provides a summary of the top 500 communities. The remaining rankings are not revealed as the intent is to identify excellence and study it to establish models for other counties that are also working to improve the quality of life for their residents.
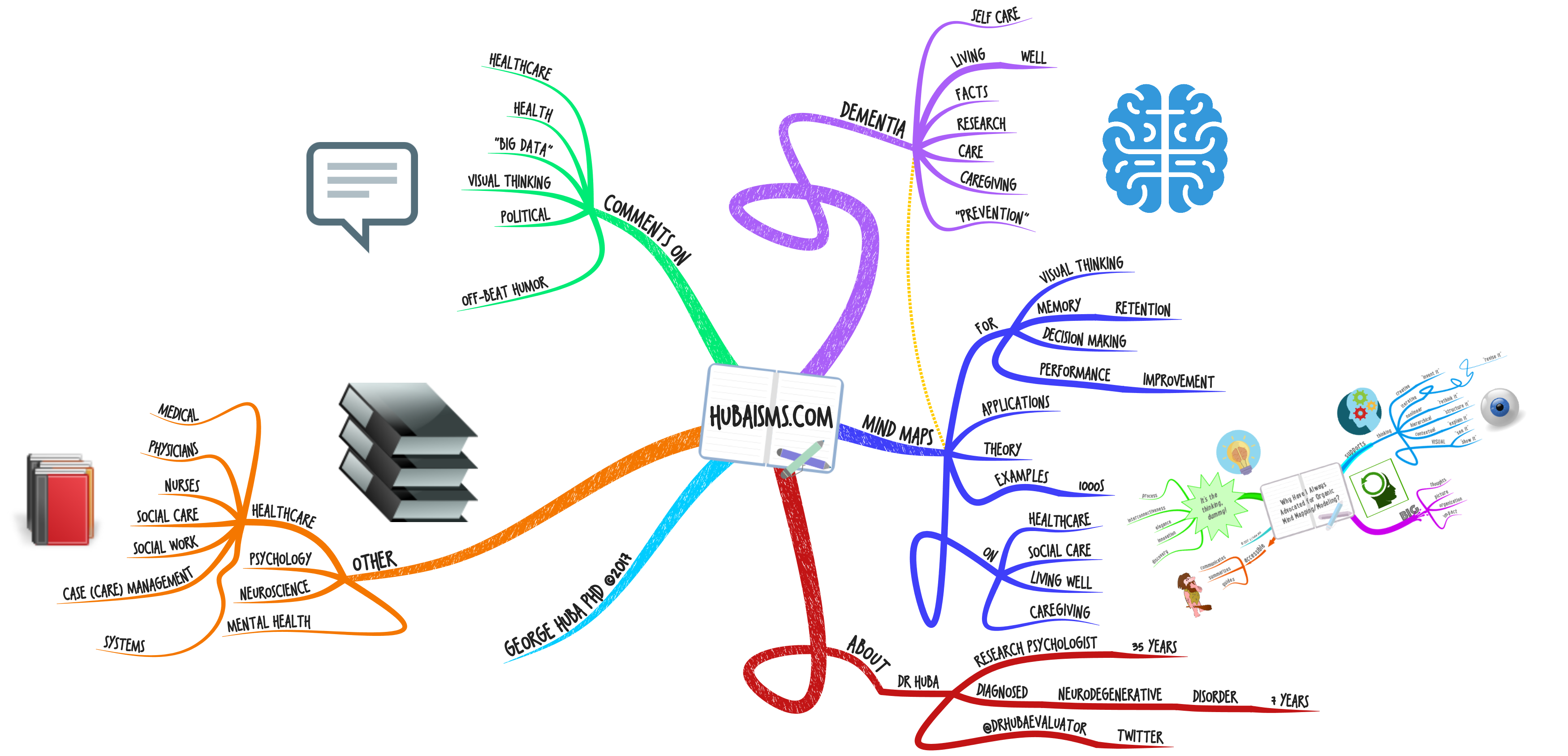
Data available on each community includes well-constructed indices of the following characteristics listed in the mind map below. Click on the map to increase its size.

I spent more than 25 years in my post-doctorate career studying the health of communities throughout the USA, including a) small “frontier counties” too small to be considered rural where there were 5 times as many cows as people and the trip to a doctor was more than an hour for more than 50 percent of the population; b) the fourth largest U.S. county in a location on the Mexican border; c) large-city neighboring “bedroom” counties; and d) healthcare systems in more than 100 other U.S counties. My work (in collaboration with my business partner Dr. Lisa Melchior and our staff at The Measurement Group) was primarily focused on developing high quality, effective, and accessible care and treatment for people with mental health problems, drug and alcohol abuse and addiction, HIV/AIDS, extreme poverty, unstable families, inadequate or housing, poor education, immigration status, criminal justice system involvement, dependence on public-supported health- and social-care systems, and legal unemployment with a subsequent dependence upon “illegal employment” such as selling drugs and sex work in order to support themselves and their minor children.
Dr. Melchior continues our work.
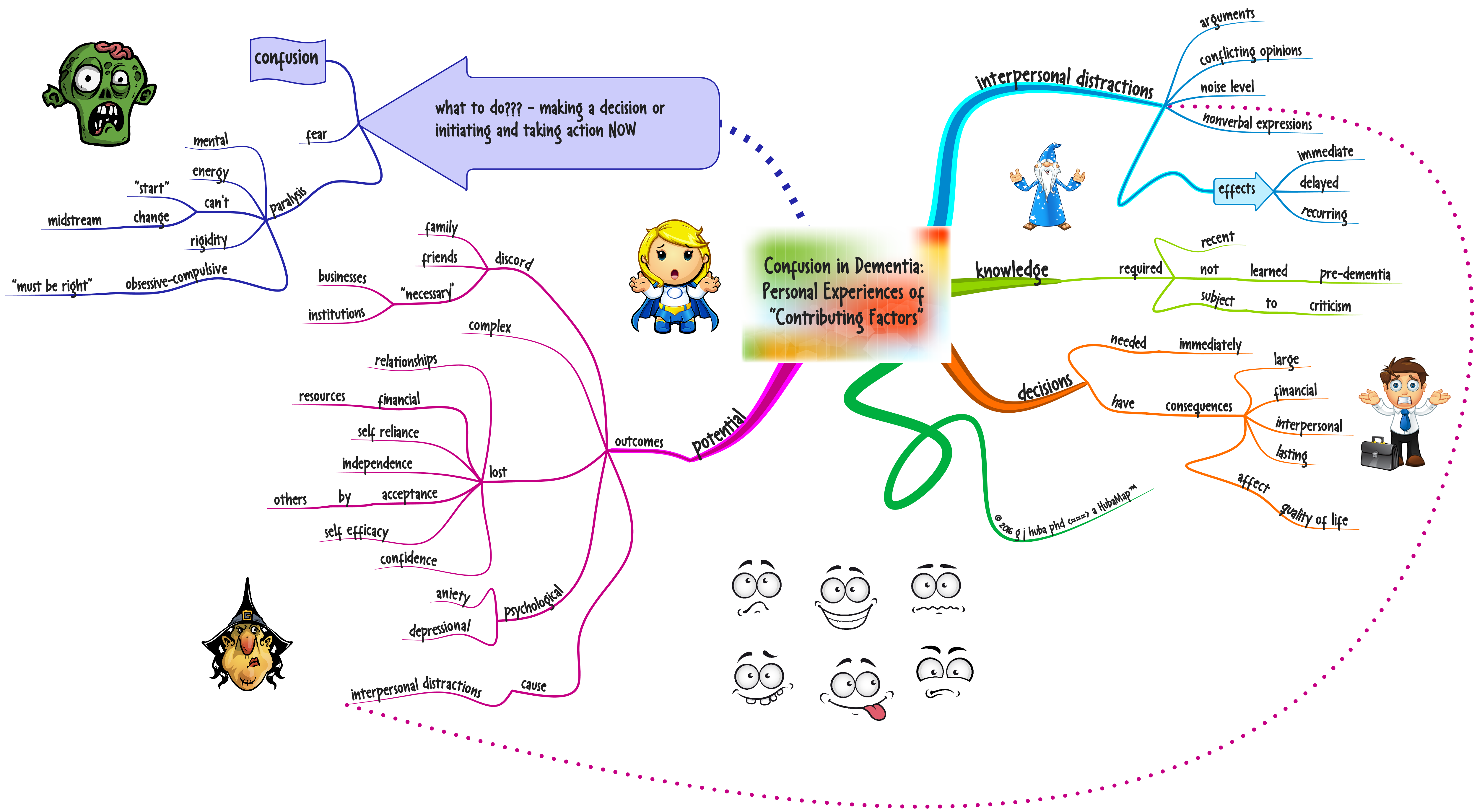
As we worked with health systems and clinics, what I concluded was that a very comprehensive service system with widespread support among residents, service providers, and elected officials was necessary to make a community healthy. It was clear that all of the major stakeholders in the system need to communicate clearly to the other stakeholders about what they could and could not do with available resources. Stakeholders needed to learn to how to leverage their resources with those of other stakeholders to provide better services for a lower cost. A permanent system of making decisions and sharing resources and improving services needed to be formed and nourished.
The basic components of our work included assembling data from sources such as surveys, focus groups, interviews, and public databases. We presented these data to groups of stakeholders and facilitated discussions on how various systems such as healthcare, public housing, law enforcement, and education-training could work together and share resources. Progress was monitored and evaluated and new cycles of data gathering, communicating, discussions, and program alterations were conducted.
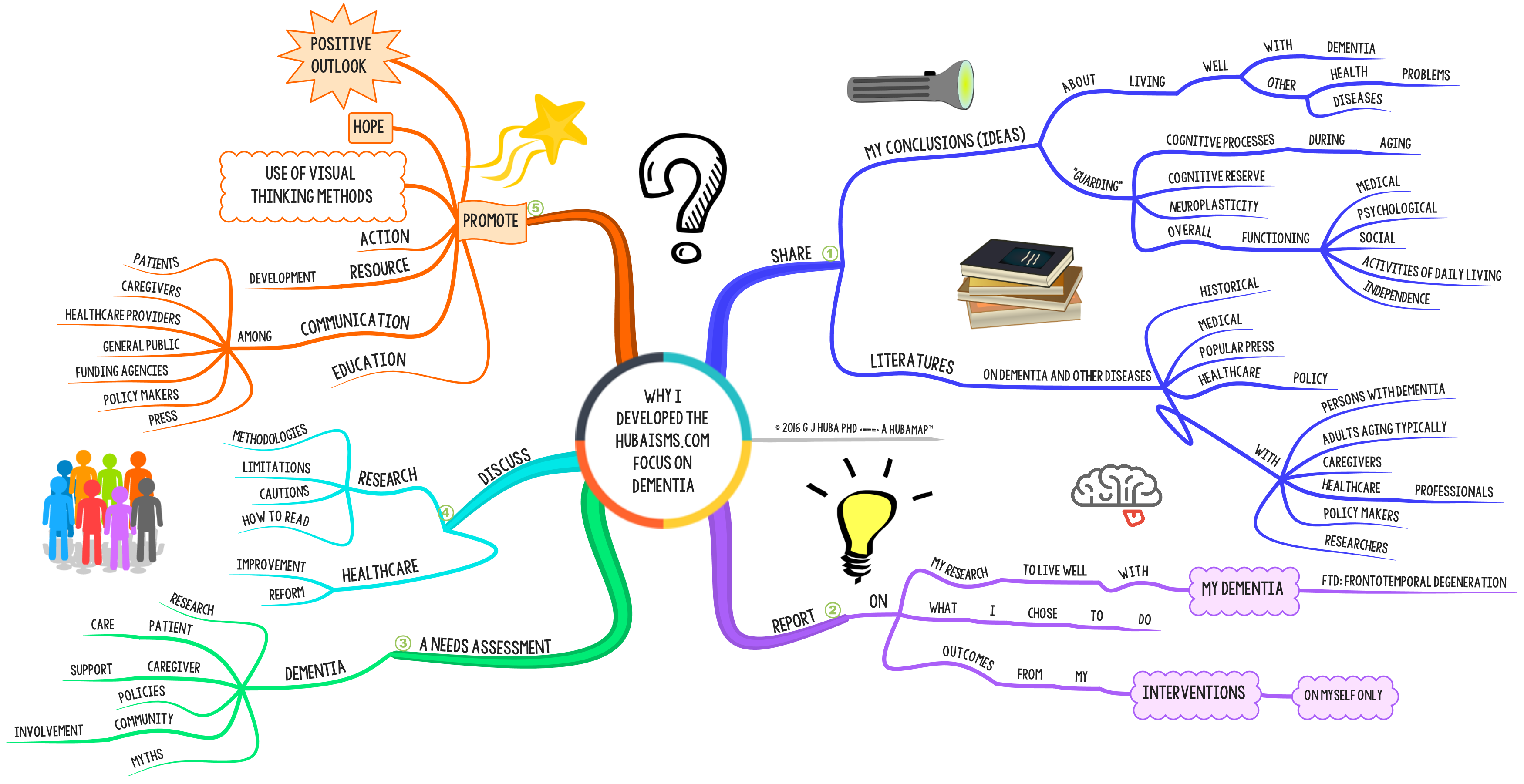
The following diagram shows the steps our process went through in order to build a self-sustaining system of interdependent services and joint decision-making in order to make a community more healthy. Click on the mind map to increase its size.

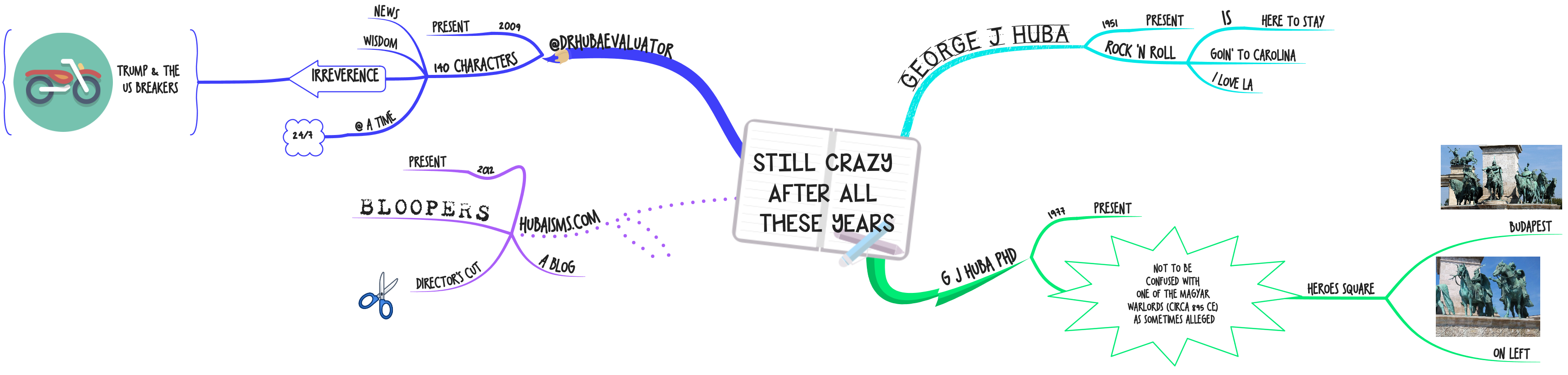
It is often said that “it takes a village” to plan and implement long-lasting improvements in a community. It does, but it takes a few other things also as well. Click on the diagram to increase its size.

Like this:
Like Loading...