People with Dementia who blog, write, speak at events for healthcare providers and caregivers, or tweet can be a powerful force for improving public and professional understanding of dementia.
While I was trained as a psychologist and other bloggers with dementia also have advanced healthcare degrees and experience (@KateSwaffer of Australia comes immediately to mind), many truly excellent bloggers talking about their own experience have little experience in healthcare, social care, or research.
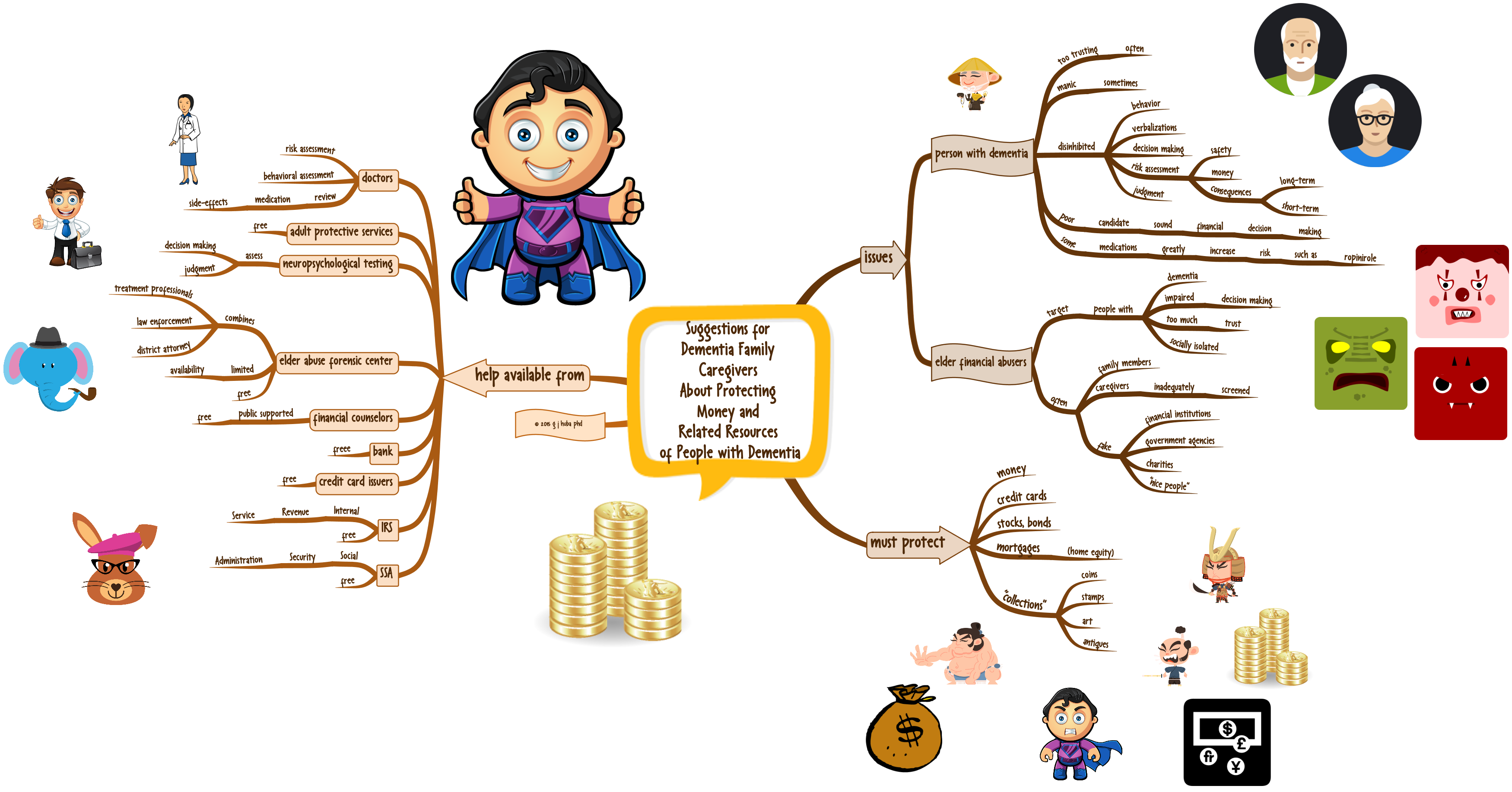
Personally, I wish that there was someone who would look over my blog posts to ensure that they medically accurate, use the names of pharmaceuticals and diagnoses correctly in accordance with current terminology, and reflect mainstream positions.
If some advanced medical students, advanced psychology and social work graduate students, advanced practice nursing students, and others were available to quickly review short blog posts, the information going from people with dementia to others (including both other people with dementia, healthcare providers, and caregivers) could be greatly improved.
Rewriting is not needed. Simple fact checking is. Blog posts are usually short, and probably some simple fact checking could be done in five minutes or less. And yes, a waiver should be signed so no volunteer can be sued.
A suggestion. I do not have the energy to make this work, nor the appropriate expertise. I would love to see someone take this on as a project.
George