December 22, 2022
Posts tagged mindmap
Choose another tag?
The Only Way (Without Vaccines) to Fight COVID-19 Spread is With Behavior Change Methods and Support Services. Stop Being Dumb and Provide Them.
No covid vaccine yet. Even if one were to be fully tested and proven safe and effective tomorrow, you probably could not get a shot until 6-9 months later.
Mask use seems to be topping out at around 70% in the United States and even conscientious mask wearer and social distancers are getting pandemic fatigue and less conscientious about always using protective behaviors.
The USA is not using behavior change and social support methods to help deal with unhealthy and potentially virus-spreading behaviors.
Instead of promising a vaccine and telling me to wear a mask, how about some social support methods to help with people feeling the depression and anxiety and hopelessness and fatigue and loneliness that comes during a pandemic. Most Americans could use some support in dealing with the balance between working and providing childcare/homeschooling. Or the frustration of being alone at Thanksgiving.
How about promoting behavior change and showing people how to get a mask to fit comfortably and correctly, or showing people how to judge they are six feet away from others. How about getting cigarette smokers to stand 12 feet away from others as they do the huffing and puffing thing in service to nicotine addiction.
A lot of people would benefit from counseling and group support-self help groups during a pandemic.
Many need a case manager to help them get food or a place to live or a job or child care or eviction or mortgage default. Others may need a legal counselor to help deal with problems incurred because of wholesale job loss and the resultant loss of life savings.
To stop the spread of COVID-19 you cannot just tell someone to wear a mask or not go to a family member for support.
What you need to do is to help individuals with pandemic fatigue and other problems find ways to constructively deal with the pandemic and get help from public sources.
Fortunately, most of the social services needed to help many people deal better with the pandemic can be provided by trained mental health and healthcare professionals and their assistants. When provided by telephone or video sessions or online support groups and counseling or specific advice to someone getting evicted these services are much less expensive than treating someone in the hospital or outpatient clinic who has become infected with COVID-19. And of course, every person who gets COVID-19 can potentially die or be affected by lingering symptoms for the rest of their lives, and the cost of any life or development of a lifetime disability is one we should try to avoid as completely as possible.
If we want to cut the levels of COVID-19 we need to up the prevention, support, and behavior change services we provide.
Click on the mind map to expand it and look at the issues in providing behavioral and support services that could make it easier for people to avoid dangerous behaviors that spread the disease.
We All Age — Try Delaying the Inevitable with Visual Thinking Methods: A Mind Map
Mind maps and related methods can help you use visual thinking to fight against cognitive decline and dementia. These methods can also help you maintain physical and mental health by maintaining control, making good decisions, remembering key information, and planning. Or, maintaining self-sufficiency, control, and independence so as to retain an acceptable quality of life.
Click on the mind map to expand it.

How Psychology has Failed Persons with Dementia [by a Psychologist with Dementia]
by George J Huba PhD (Psychology)
This weekend the American Psychological Association is meeting in San Francisco. While certainly not exclusively so, the meeting tends to be dedicated to the presentation of fairly trivial and limited scope, poorly designed research studies.
Psychology should be embarrassed that the focus of the meeting is not developing new and better ways of addressing psychological problems. For instance, I have dementia. So do many millions of people worldwide. At this psychological meeting, there is little focus on actually improving the lives of persons with dementia. The same is true for many other psychological disorders.
How has psychology failed persons with dementia? The following mind map presents my assessment of the situation.
Why does psychology fail persons with dementia? I believe it is because the field wants to pretend it is a science of the rigor of biology and physics, rather than focusing on becoming an evidence-based way of developing better ways of patient assessment, screening, treatment, and communication. What a waste. And remember that I am a person with degenerative cognitive and behavioral disease and I get it. Shame on psychology.
Click the image to expand it.
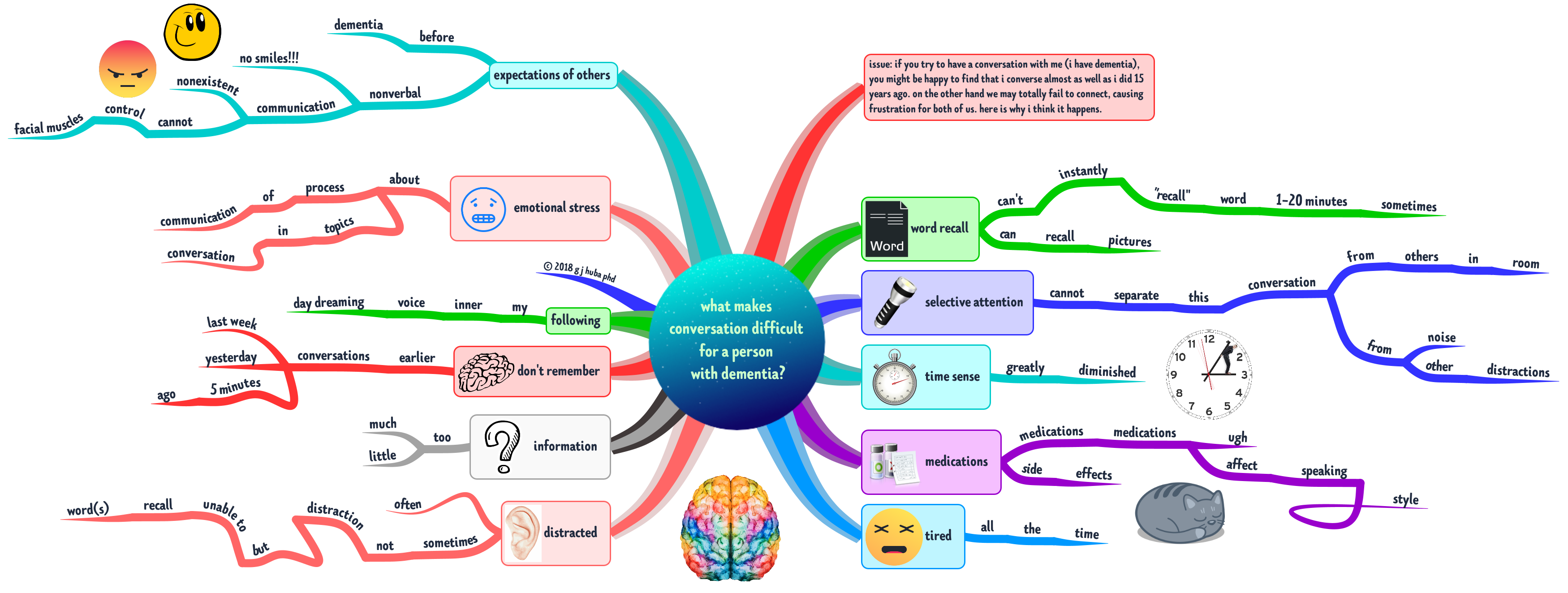
What Makes Conversation Difficult for a Person with Dementia?
by George J Huba PhD (Psychology)
Dementia is a time that gets extremely complicated for a person with dementia and their spouse, family, friends, new social acquaintances, healthcare providers, and caregivers.
Probably the biggest issue is that those who interact with the person with dementia expect the PWD to communicate in a way that is diminished but still like the way a typical person without dementia communicates just now at a lower level.
It is difficult to communicate with a person with dementia because their own experience of communications is now shaped by the brain changes and other symptoms of dementia. What about your Mom who no longer smiles when you say something she has always liked or when you bring her the pistachio ice cream she has always loved? Ever consider the possibility that she thinks she is smiling but has no control over nonverbal communication such as her smile. Brain damage of various types can cause the loss of nonverbal communication abilities or control of facial muscles.
Why does your friend always get overwhelmed and say something stupid when there are lots of other people around? Perhaps they can’t focus on what you are saying because there is so much noise and motion from distracting sources?
Ever wonder why your friend with dementia comes back with an answer to a question five minutes after you asked the question? Brain changes and damage during dementia may make it hard to retrieve information or think and a loss of a sense of time may mean your friend keeps working on answering the question long after the conversation has moved on.
In dementia, a daydream may be as vivid as something in the real world, and just as distracting. In dementia, you can’t deal with too much information because it distracts you and can’t “fill in the blank spaces” if you receive too little because your “executive functioning” has been destroyed. You tend to get anxious during a conversation not only from unpleasant topics but also from worrying so much about missing a word or forgetting a name or misinterpreting a suggestion as hostile when it was just a normal joke.
The physical and psychological consequences of dementia combine to make it seem that a person with dementia is speaking a different language. They are.
And yes, those 20 or more pills the person with dementia may take daily can affect the ability to speak clearly, pay attention, be sleepy, look like they are bored when they are not, or become even more anxious.
Additional thoughts are arranged on the mind map below.
Click on the image to expand it.
Always try to remember that the person with dementia is often not disinterested or misunderstanding you or too tired to think or extremely distracted in what you think is a peaceful environment.
And if you are a person with dementia, remember that your friend is not trying to mislead you or express hostility and disapproval. They are not trying to trick you or harm you or pick a fight. You might not remember a conversation your caregiver says you had 10 minutes ago, so get over it and trust the other person. Nobody is criticizing you as a person because you can no longer tie your shoelaces or your necktie.
All parties in a conversation with a person who has dementia need to realize that the “rules” for the social encounter have changed because of the disease. Both persons with dementia and their families and friends and caregivers need to realize that is just as hard for all parties to figure out this new “language of dementia.” But it can be done and when mastered can liberate everyone to some degree.
Learn to laugh and smile and enjoy the company of each other again. The positive emotions are still there but they may have to be expressed in different ways. Learn how to express oneself when one or more parties has dementia. It’s worth the time. For everyone.
#mindmap #mindmapping #dementia #Alzheimers @DrHubaEvaluator
how to think differently (= BETTER) when you have dementia
The #1 thing that I have learned over almost a decade of living with dementia is that thinking in pictures (images, diagrams, doodles, etc.) is much more effective than using words alone. Hedge your bet. Use pictures that associate with words rather than just words. After all, in many types of dementia, you lose your words at the end while the pictures may escape loss.
Try it. You will probably like it. Creating visualizations of important events, ideas, feelings, and other information can be FUN.
I’ve been using visual thinking methods for the past 10 years. They work (for me).
Part 01: Six Years of Fighting My Dementia with Visual Thinking – Activities
If you have not read the Introduction to this series of posts, it is important that you read it before this post. Click here for the Part 00 Introduction. This post is part of a series of more than a dozen posts.
I worked on understanding health and social service programs, especially for the disabled, poor, disenfranchised, and traditionally underserved as a program evaluator for about 25 years. I was very good at it and worked with hundreds of programs spread over most US states.
In writing about my activities to achieve stability in my dementia and maximize my quality of life, I am going to employ the tools of program evaluation to describe what I was trying to achieve, what I did to achieve my goals, why I did various activities, and which parts of my interventions seemed to help me the most. No, not in this post but in a series of more than a dozen posts.
In this post I will start by describing the activities I designed for myself and did throughout my period of diagnosed dementia over six years of living with the disease. In subsequent posts, especially Posts 02 and 03, I will discuss the outcomes of my activities. After that, I will address some of my activities — and especially those that “worked” extremely well for me — and describe them in depth, show how other individuals might use these methods, and how dementia caregiver and healthcare systems might be built around them.
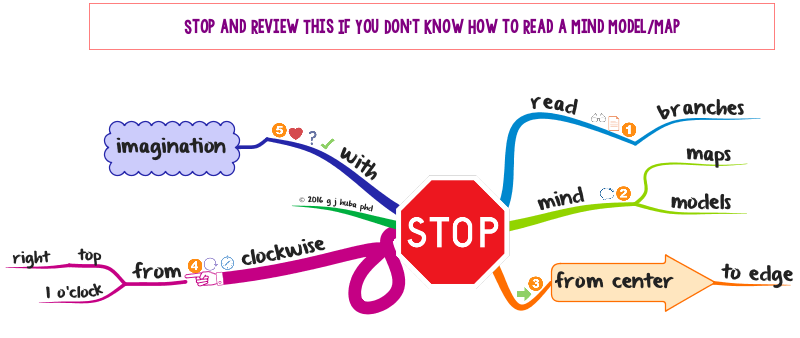
The image below is a mind map. Should you not be familiar with how a mind map is drawn and read, please search this website for posts on mind mapping using the search box. Or, go to the home page by clicking here and look at the list of pre-defined searches.
A very simple set of rules for reading a mind map is as follows.
- Start at the center of the diagram. Each of the topics (ideas or major branches) that come out of the center represents an issue. Important information about the main issues is given as a series of branches. The organization is in an outline or tree where large branches divide into smaller branches and smaller branches divide into even smaller branches.
- Think of the map as a clock face and start at the 1 o’clock position (upper right corner). Read outward from the center along the branches and sub-branches to see how ideas and information about the topics can be arranged in a hierarchical or tree structure. [If you could go up a huge fire truck ladder and look straight down, you would see a structure of tree branches that looks like a mind map. When we study or read a mind map, we are looking at a whole tree — set of information — and then seeing how small and more specific information spreads from the trunk.]
- Go around the map in a counter-clockwise manner (to 2 o’clock, 3 o’clock, etc.), following the branches down to their branches and their branches and finally to twigs. Remember that we are looking down at a whole idea [or tree] and its branches and their branches in order to understand how the information represented on these branches goes together and what the most important information is.
- The mind map is thus a picture of major ideas followed by its major subdivisions or branches and sub-branches. The “big ideas” are attached directly to the central issue.
- A mind map is a way of showing in an image how a set of data pieces or ideas go together.
- The pictures, color coding, and fonts are used to designate what is the most important information in the mind map. When you are trying to remember or organize or determine priorities, the pictures, color coding, and size of the fonts can help you store information in “visual” parts of the brain and then retrieve it by thinking about pictures, the color coding, or size-importance of the information.
Click on the mind map to expand its size and zoom to various portions of the map.
As you can see, I tested app after app after app on my Mac and iPhone to see which could help me. I read all about how to mindmap and draw sketchnotes and I practiced and practiced. I learned to read “dog” and taught my Newfie to understand “people.” I doodled, watched the news, built a highly-rated social media following of more than 140,000 individuals interested in healthcare, dementia, visual thinking, and 100s of other topics from around the world. I went to concerts, watched movies, and cheered for the two local universities with huge sports programs. I engaged some new parts of my brain. I thought in pictures.
- I HAD FUN.
- I LEARNED MANY NEW THINGS THAT STRETCHED MY BRAIN INTO NEW CHANNELS.
- I BUILT COGNITIVE RESERVE.
- I THINK I PROVIDED NEW INFORMATION TO PERSONS WITH DEMENTIA AND COGNITIVE DECLINE, CAREGIVERS, HEALTHCARE PROFESSIONALS, AND THE GENERAL PUBLIC. I FEEL GOOD ABOUT THIS.
- I HAD FUN.
Stay tuned, the interesting stuff starts next.
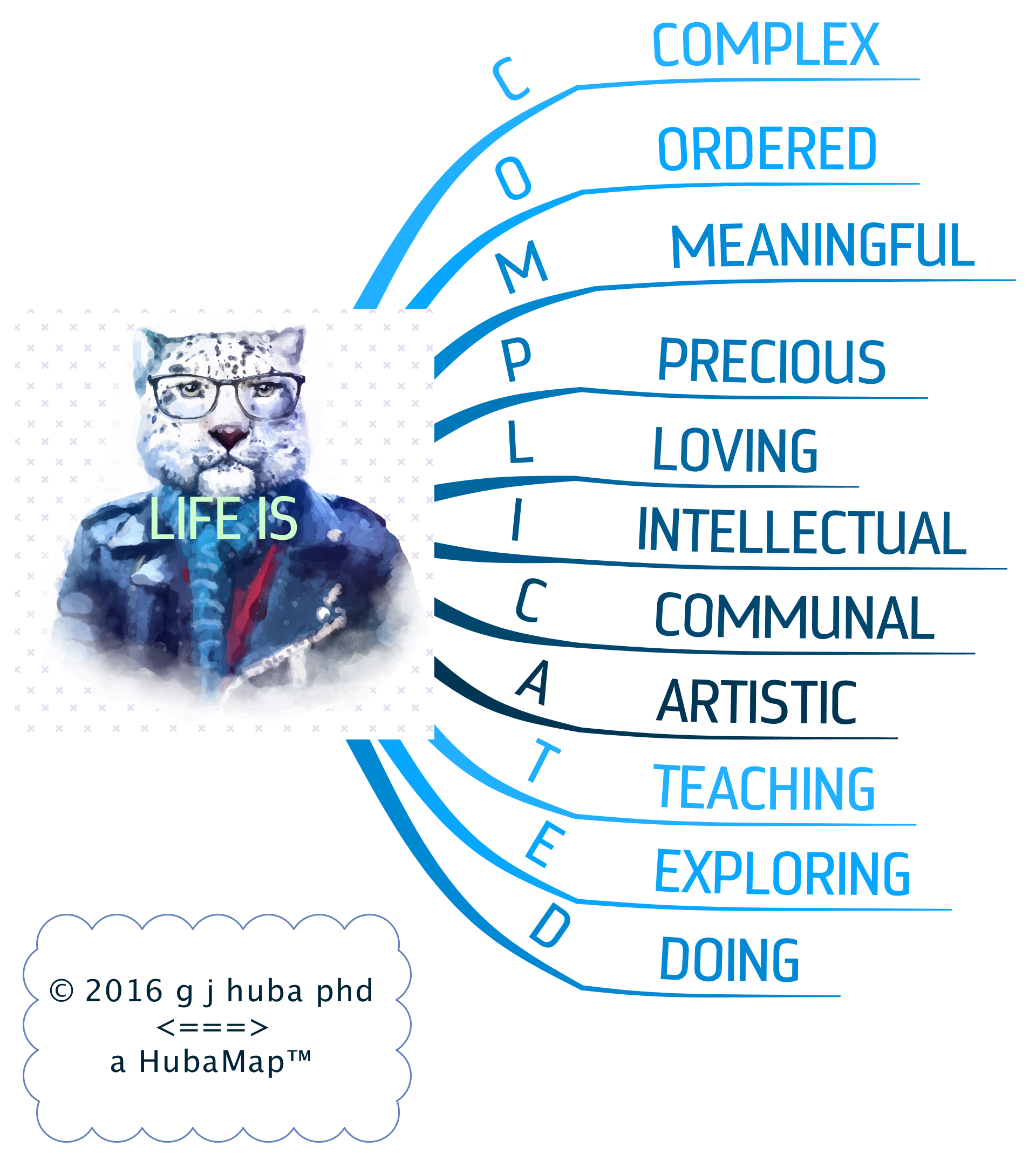
CODER Algorithm for Mind Mapping, Revised 2017
WHY I MIND MAP…
Since 2013 when first presented, my CODER algorithm has been one of the most accessed posts on www.Hubaisms.com. Recently it has been “rediscovered” and is now being accessed frequently.
So I decided that I should take a look at it and see if it needed to be upgraded. In fact, I discovered that my views were about the same on how to develop a meaningful and informative mind map. Consequently, I just made a few very small and largely inconsequential content changes to the map.
The map has been reformatted. The program in which this was originally drawn (iMindMap) has been enhanced significantly and annually since 2013.
The original mind map from 2013-2015 can be accessed HERE The original post includes textual material about the map.
Drum roll, please. Here is the 2017 revision. Click the image to expand it.

DementiaCare Services Needed in ANY Revised/Replaced US Healthcare Plan
ObamaCare revised/enhanced?
Trump/RyanCare another draft not submitted to Congress?
Within the extant and mythical healthcare plans, additional dementia care services need to be included. Most are cost-neutral or may actually save money while providing better patient outcomes.
Case Management makes existing healthcare services (doctor visits, medications, emergency care) work better. At a very small cost that should actually SAVE money, case management can provide better total patient care, cut unnecessary emergency room visits, and achieve better medication outcomes. What isn’t there to like?
Dementia Caregivers are most often UNPAID, female family members forced to juggle their own jobs/finances, families, and general lives to care for a loved one. Support is required for Dementia Caregivers in the forms of training, support, advice, and FINANCIAL COMPENSATION for their services. They do the work, they should get paid for their time. An upgraded system of paid family caregivers should make DementiaCare more effective and reduce other costs in the healthcare system to such a degree that it will be cost-neutral. An unnecessary hospital stay or emergency room visit can cost as much as $10,000 — $20,000. A family caregiver could be paid for 500 hours at $20 per hour for $10,000. Train family caregivers, pay them, and you have a cost neutral system. What isn’t there to like?
Mental Health issues often lead to huge patient distress, anxiety, and medical management problems. They can frustrate caregivers and lead to nonadherence to medication recommendations. Therapy and counseling can help patients and caregivers as well as cutting overall medical costs. What isn’t there to like?
Group Adult Daycare can provide needed respite for family caregivers as well as important social and recreational experiences for patients, thus enhancing their lives and to some degree ability to function independently. What isn’t there to like?
The following mind model provides some details. Click the image to expand it.
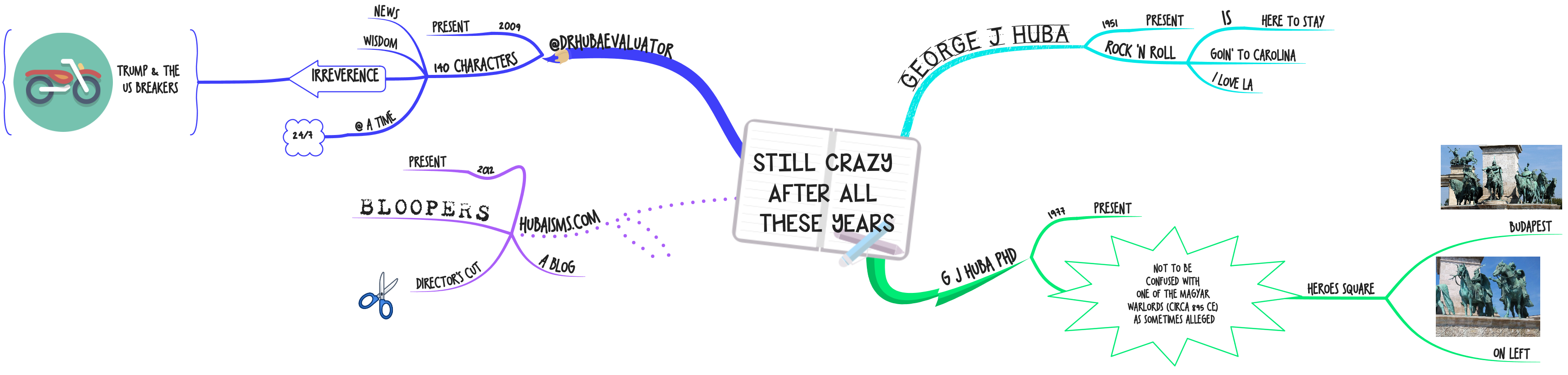
A Cognitive Strength Useful in Living with Dementia is Apparent Processing News
I get in trouble when I make mind maps about Donald Trump. This is a mind map about processing repetitive TV cable news (on CNN and MSNBC and FOX) about the most televised story — Donald Tackles the USA and the World — at this point in late April 2017.
Mr Trump is just completing the first 100 days of his Presidency having accomplished less — according to the fact checkers from numerous news organizations — than any President since the index has been tracked from the beginning of Franklin Roosevelt’s Presidency in the 1930s. Mr Trump believes he has accomplished more than any president ever studied in his first 100 days.
I am a lover of news stories where the President gets bashed on TV. In the 1970s I watched (and read about) all the hearings focusing on Richard Nixon and Watergate. In the 1980s I watched huge amounts of TV about Reagan and Iran-Contragate. In the 1990s, I watched the hearings about Bill Clinton and the blue dress and impeachment and not inhaling. Nothing of a comparable nature occurred during either Bush presidency or that of Barack Obama. I almost didn’t know what to do with my spare time.
Now, I am watching numerous hours of TV/video on the major USA news channels (including CNN, MSNBC, Fox, CBS News online, New York Times, Washington Post, and of course the best news outlet for all news worldwide, BBC). And even ESPN has had a big Trump story about star players declining invitations to the White House to meet POTUS.
My dementia has been progressing at an ever increasing speed in a downward spiral during the past months. I remember (recall) less from current events and “work” and daily tasks. When I can retrieve information I do so very S—L—O—W—L—Y. Judgments are tougher, understanding sequences are harder, and writing down what I think is very slow as the length of my current journal entries (and al of the wurds nat spelled wrongly or too bigly) is increasing grately. Handwriting does not come with A spel chkr.
The current trend in cable TV news on MSNBC and CNN and others is to have one-hour shows where a moderator/commentator discusses all of the “important” news of the day with 2-5 different “self-styled” experts ranting from all political persuasions.
7 hours of liberal rantings about Trump is available on MSNBC and to a lesser degree on CNN; Fox News has 7 hours of conservative rantings about how terrible it is that the liberals are ranting about Trump.
I have repeatedly argued that inexpensive (or even free) visual thinking/mind modeling methods can help a person with dementia “rewrite the operating system” on that storage device we call the brain and think better, albeit in a different way.
As I was making the following mind model (AKA mind map) about Trump’s first 100 days yesterday, I was struck by how rapidly I could create this fairly complex model. I think it shows that the intrinsic interests and REPEATED exposures to structured, summary information can be well captured using visual thinking methods by a person who has lived with dementia for more than half a decade after diagnosis. While I understand that 40% of USA voters will find the content WRONG because it is very liberal rather than very conservative, I do propose the hypothesis that developing a fairly complex, fact-based mind map of current news shows the value of mind mapping for someone with dementia basing this conclusion only on my own experience. And it works no matter what you think about Trump.
I hope that as many conservatives as liberals will use these methods to study the facts of issues and their own conclusions and evaluate the completeness of what they know.
Examine your memories and conclusions in mind models. Political leanings and party do not matter because your mind model is for YOU as much as my mind model is for ME.
Should you find my political points to be in error, just use this as a template about what you would like to say about, for example, Hillary Clinton or a Democrat in Congress.
But remember that models like the one can be developed by a person living with dementia like me.
And most importantly, I hope that we — whether your political views are similar or dissimilar to mine — can come to an agreement that cognitive methods for supporting thinking for those with or at risk for dementia belong in the next version of ObamaCare or TrumpCare along with training, support, and respite services for unpaid dementia caregivers and especially COVERAGE OF COMPREHENSIVE HEALTHCARE FOR ALL AMERICANS.
Click on the image to expand it.
Oh … and let’s make sure that no President of any party ever uses the nuclear option. I hope we can all agree on that.
Are the Dementia Care Mind Models (aka Mind Maps) on Hubaisms.com Useful with Other Diseases?
The title of this post is the #1 question (comment) I receive on Twitter when I make a post about content on this site.
The answer to the question is a guarded yes. Most (in excess of 85%) cover basic issues in caregiving, healthcare, patient management, note-taking, self description, cognitive issues, case management, family management, and resources within the healthcare system. Some is specific to dementia (mind maps on types, treatments, research, experiences of those with dementia).
My expertise, research and personal interests, and personal theories derive from within the context of dementia in terms of my professional interests, experience as a caregiver for my mother and grandfather, research, test development and personal experiences. So I always present my ideas targeted toward persons living with dementia, their caregivers and medical providers, dementia care/case managers, and those adults concerned with improving and or maintaining their own cognitive skills or preparing for cognitive decline.
There are many applications of my ideas to many chronic and acute healthcare conditions. Caregiving issues are in many cases the same, healthcare management of different conditions may be fairly similar, and nobody has enough resources to do what they actually want to do.
Where I have great reservations in applying (or extending) my ideas about cognitive skills and quality of life is in understanding and intervening in cognitive and the other medical, and mental health issues of children and adolescents. ADHD, adolescent suicide prevention, youthful problem behaviors, dyslexia, and many other conditions require very specialized professional training. Caregiving by family members and paid trained-paid caregivers often requires different skills, knowledge, and emotional supports than it may for adult patients. While many trivialize the issues and state that declining older adults are like children, such a statement makes minimizes (in a way both pathetic and potentially dangers) the very real and large differences in the care of these groups at either end of the age spectrum.
NO posts or mind models in this blog are specialized for the very real unique needs of children, adolescents, and sometimes younger adults.
Click on the image to expand.
Conditions Under Which the Impact of a Mind Map is Maximized
Want information you created or curated to have the greatest impact? Then put it into a mind map. Not a mono-toned mess of straight lines at right angles but curves with colors and an organic style. A mind map utilizing rules that follow what is fairly well known about visual thinking. A mind map like the one below.
Click on the image to expand it.
Huba’s Review of the iMindMap 10 Program for Mind Mapping
NOTE: Version 11 OF iMindMap was released the first week of May 2018. At this time (7-1-18) I have been using the program for about two months. I will have a full review posted within a week or two. As a brief note, Version 11 includes a number of enhancements. The program remains the best one for mind mapping and the updates made from Version 10 to 11 are significant and worth the upgrade price.
I doubt that there are many people expert in mind mapping who would disagree with me that iMindMap is the most feature-laden of the more than 100 programs for mind mapping to be found all over the Internet.
Once a year — as promised when the program was first introduced — iMindMap has a new release that provides many new features and usability enhancements. And unlike others, they produce a great upgrade every year on time. And free from most bugs that live in Cupertino and Redmond.
How good is iMindMap 10?
Click on the mind map (actually mind model in my terminology) below to expand its size. For those of you with no patience or dramatic sense of the big build-up, you can skip directly to the “9” branch. iMindMap is the 8,000-pound gorilla.
As a note, my review was conducted about six weeks after receiving the program and using it exclusively rather than earlier editions. I use a Mac only, and my review was conducted on a 2013 MacBook Pro. I have worked with the program both on an internal 15″ retina MacBook screen and a 27″ external monitor. [I actually like using the MacBook screen rather than the larger desktop monitor.]
Chris Griffiths and his team at OpenGenius have taken the work of Tony Buzan and in the process of developing a program expanded and formalized that conception in a creative way that is brilliant in its overall utility and ease of use. iMindMap 10 is my favorite mind mapping program, but most importantly my favorite and most useful thinking tool. For those of you who do not follow my blog in general, I live with Frontotemporal Dementia and iMindMap has served as a “brain assistance tool” for me since 2010 in daily living and in continuing my professional interests in a creative way. I can accurately say that the various versions of this program “changed my life.”
This is a tool formulated by expensive consultants who want to help corporations make more money while at the same profiting from that help. But the tool has come to greatly exceed the original vision and is intuitive to use and most adults and all children can learn to use the program for free using Internet trainings. Don’t be scared off by all of the publicity about a $3500 training and a certificate signed by a consulting firm (not an accredited educational institution). You do not need a course to learn this program and it is not clear to me that expensive courses help you learn to apply this program in the real world. If you are willing to invest a few hours you can be doing adequate mind maps; if you invest 10-20 hours you can be doing accomplished mind maps.
Get over the hype and realize that you CAN learn this program quickly on your own and even more rapidly if you study examples available without cost at many blogs including this one (Hubaisms.com), a depository of many thousands of mind maps at Biggerplate.com, and many other sites including youtube.com where many training sessions are presented.
While there are four “views” in this program, the primary mind mapping module is the reason for using this program. The other three views are largely alternate ways of looking at the same information and data. While they may be “quicker” ways to collect information together from a lecture or library research, at the end they feed their data into the mind mapping module where the actual thinking work, theory building, model development, and communication is done.
I have a few criticisms of the program, but these criticisms do NOT change my overall rating of the program as A+.
- The time map module is really just a Gantt chart of interest to but a few mid-level corporate managers and high level executives who have not yet adopted better ways of team management. As a Gantt chart the module is fine, albeit about the same as most existing software in that area. Unless you are like a friend of mine who manages 10-year projects to send landers to Mars with 10,00 team members, I cannot imagine why you would want to use a Gantt chart.
- In my view and that of many other potential users, a “time map” is actually a timeline that incorporates mind map features. While others have tackled this issue (most notably Philippe Packu and Hans Buskes), my formulation was the original. The resulting blog post (click here for a new window) has been the most read one about mind mapping methods on my blog site for FOUR years. I’d urge the iMindMap developers to look at my model of time maps which requires a lot of custom work that I am sure they could easily automate.
- For almost all mind map users, the future is using pre-made templates designed by content experts. Purchase a template package and then you can then create your own mind maps by adding your information to the pre-designed expert map for your area whether it be healthcare or project management or writing a term paper or designing a research project or selecting the right clothes for a 5 day business trip. At this time iMindMap does not yet have a way of protecting the intellectual property of template developers which provides little incentive for developing templates as a business and therefore stunts the growth of the mind mapping community.
- For this program and all of its competitors, the icon and image libraries are never big enough. On the other hand, you can purchase separate icon and image sets from third-party packagers on the Internet if you have special image needs. iMindMap allows you to use such external pictorial elements extremely easily. My favorite new feature is that you can add icons to their library and size the icons in a custom way. iMindMap’s included images should more fully capture the fact that users of mind maps and their audiences are much more diverse in terms of ethnicity, race, gender, gender-orientation, education, and age than the included image libraries. And hey OpenGenius folks, how about some icons for numbers in colors besides orange and lime so that the color schemes of my mind maps are not destroyed if I number ideas.
- More free online trainings would be desirable, and most importantly trainings that do not run at the speed of a bullet train. Two minute presentations that cover 20 minutes of material are somewhat counter-productive. The current videos run too fast for new users and at time for even the most experienced users.
- My experience — admittedly infrequent — is that Technical Support is fairly “rigid” in that there are lots of forms to fill out before you get a real chat session going and too many requests to send them esoteric files on your computer. All in all, as technical support goes, while everybody is trying quite hard to be helpful, they ask you to conform more to what is convenient for them than what a confused user can deal with. When I want help or to make a suggestion or make a request for a new feature or default, I want to just compose a short email so OpenGenius can get the right person there in contact with me. I most definitely do not want to complete an overly complicated form. Too much technocracy in that process.
- Besides the books of Buzan which are not all that useful for learning the program or how to do real visual thinking in real world applications other than rudimentary management, OpenGenius needs to develop some easier access, very practical books that act as “manuals” and present information in more comprehensive ways than is done now. Old fashioned manuals that are (or can be) printed have a lot of appeal to many.
In summary, this is an amazing program that is much more than a program for mind mapping. It is unsurpassed among mind mapping programs. Additionally it is what I call a “visual thinking environment” or VITHEN. My “criticisms” are minor and do not in anyway diminish my overall evaluation of the quality of the program.
My blog at Hubaisms.com on which you are reading this review was designed and “written” largely in “iMindMap.” Most of the mind maps I use to guide my own “complicated” life were developed in iMindMap.
Exemplary job folks at OpenGenius. Version 10 is an additional large step in the evolution of the program and mind modeling.
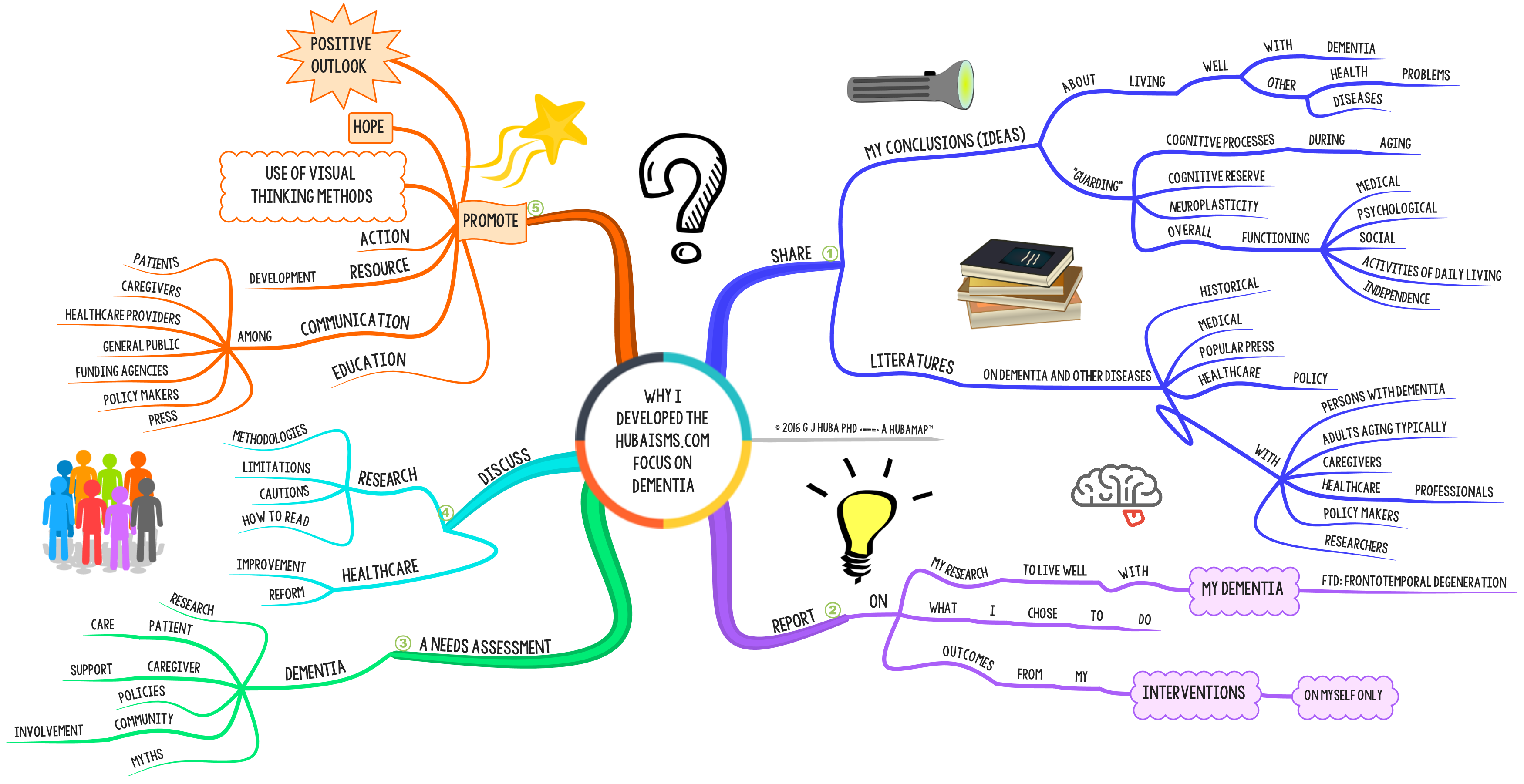
The #Dementia Focus on Hubaisms.com [My Vision, Part 1]
The mind model (aka mind map) below discusses my vision in developing the dementia focus on this website. I started to build the web site about two years after being diagnosed with a neurodegenerative condition (2012). Thus the entire blog is the work of a developer experiencing dementia while designing and preparing the content for the site. The site discusses my progression through cognitive impairment and decline into dementia. More importantly it discusses how I tried to help myself coordinate and use to full advantage the support and professional expertise made available to me by family, friends, the community, my doctors, and the general world-wide of patients and professionals the major issues.
Nothing in this blog post (or any other on blog post or page on the site) is intended to be, or promoted as medical, psychological, or any other form of treatment. The ideas in this blog are about using some commonsense note-taking and visual thinking methods to possible help you live better with dementia. I tried it on myself (only) and I am encouraged although I freely admit that full scientific study is needed.
These methods and comments will not substitute for medical and other professional treatments. They do not cure dementia. They do not slow down the progress of dementia. For me, at least, the methods have sustained and increased my quality of life and I do spend more time with my family and am more independent and in my opinion think better. But my dementia is not being treated and getting better; what I propose are methods that may make it easier to independently manage selected parts of your life, be in a better mood because you are trying to help yourself, be less of a burden to your caregivers, and report better to doctor what your experiences have been since the last appointment.
Many people are miserable almost all days when they have dementia. If simple, inexpensive cognitive tools can improve some or many of those days, the development of such techniques is a huge step forward.
I hope that others will examine the information here and use it to improve the decisions they, their caregivers, and their doctors and nurses must make about their formal medical treatment.
Here is what appears in the blog posts and elsewhere on Hubaisms.com.
Click on the image to expand it.
Click here to see Part 2 of My Vision in a separate window.
#MindMapping (#MindModeling) May Promote #Mindfulness (Now and in a Future with #Dementia)
Not the past, not what might happen in the future. Fuzzy, intuitive, today’s emotions. Nonlinear, visual, big picture. Attention flows toward good, bright, happy visualizations.
Opening your mind to nonlinear thinking may provide a cognitive reserve that helps you as cognitive functions start to decline perhaps precipitously into dementia. Neuroplasticity is a mechanism that the brain will use to reassign functional processing from one area to the brain as it is damaged by trauma or disease.
One very good way to encourage the development of cognitive reserve and neuroplasticity is to practice nonlinear thinking methods that can help promote mindful solutions. Should the brain become damaged, it may be able to use nonlinear, symbolic visual thinking to cope, at least for a while. And while you practice you may also experience strength in your resolve and understanding.
Do note that the above comments are speculative. There is NO formal research on mind mapping or other comments about this in the literature (other than my own). Also, this is based only on my own experience and generalizations from my earlier research on daydreaming and imagery. So do not go about thinking that this proven. Rather it is speculative.
While I theorize that mind mapping is related to mindfulness in SOME applications, even if it turns out that it is not — from the results of formal empirical studies — there are other demonstrated benefits from mind mapping, so the actual use of mind mapping should still be encouraged.
Effective #MindModels (aka #MindMaps) for Healthcare Patients, Professionals, Caregivers, and the Public
One way that healthcare communication can be made more effective is to supplement or replace traditional pages of small-type textual information with graphic displays such as mind models (AKA mind maps), sketches, graphs, and infographics.
This post focuses on mind models (mind maps). The same general arguments would apply to sketches, graphics, infographics, and other visual information methods designed to promote a more effective patient-oriented healthcare system with more complete, accurate, and easy-to-understand information for all.
If you are not familiar with mind models (mind maps), you should look at the mind map at the bottom of the page first (Footnote).
To expand the graphics, click on the images.

Footnote
Possible “Hidden” Problems of Persons with Dementia: MindModel™
There are many problems that can plague a person with dementia. Some of these are easily detected but others may be “hidden” because of the nature of the major symptoms of the disease or “hidden” because the person with dementia (or caregiver or in some cases family members) is trying to hide some of the problems from outside observers.
For instance physical, psychological, or financial abuse will be hidden by the abuser and perhaps the person with dementia. Memory loss may make it difficult for the person with dementia to accurately report accidents.
It is important that healthcare providers, caregivers, and family members be trained to identify the hidden problems.
To some degree or another, it is likely that most persons with dementia have some of these hidden problems. For instance, I bump against things all day long, usually because I am rushing around or not paying attention because I am trying to multitask. When asked by a family member or friend where the bruise came from, I have to try to reconstruct where the accident must have happened by thinking through a lot of alternatives for a bruise half-way between my ankle and knee.
Click image to expand.
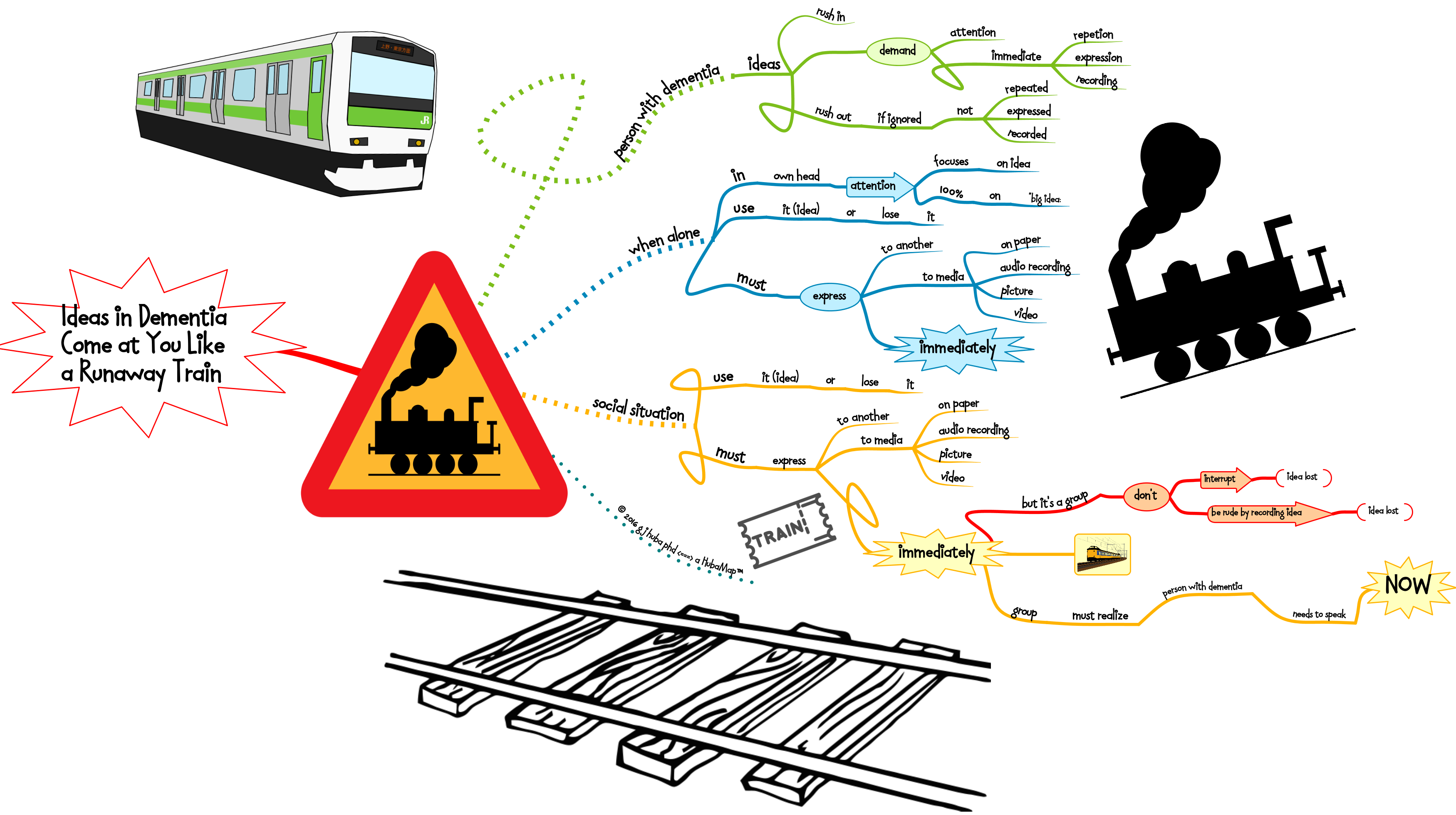
Ideas in Dementia Come at You Like a Runaway Train
A mind model (aka mind map) on the way that ideas hit you when you have dementia.
In a group, the need to say something immediately before you forget it often takes a backseat to etiquette rules of waiting for your turn to say something and not interrupting. If you are talking to someone with dementia, consider cutting them slack and letting them jump in when they can. If the group won’t let the person with dementia break in it can lead to both a sense of frustration for all and quite frankly, the loss of some good ideas and interactions.
The current rules of etiquette do not take account of the fact that some of the participants in an interaction will have severe cognitive impairment or mental illness that pretty means that if a thought is not expressed immediately it will be forgotten.
Sometimes rules need to be stretched or curved (like a railway track) and patience exercised. This is one of those times.
f I am trying to blurt out an idea to you, believe me that if I don’t say it immediately it is going down the track far, far away from me. And it may not come back for another five minutes (if at all).
Running the Race to Live Well with Dementia is Like Competing in the 10K at the Olympics
I have been a HUGE fan of the Olympics since I was a very little kid. In 1984 I got to go to the Olympic events in Los Angeles every day for two weeks, on many days with my father. That was the year that the Soviet Union boycotted the games because the USA had boycotted the Moscow Olympics in 1980. Heck, I thought it was great — the USA and East Germany (who came) won all of the gold medals! Months earlier when local pundits in Los Angeles said Los Angelenos were too apathetic to purchase expensive Olympic tickets especially with the Soviets and most of the Eastern Bloc boycotting as it would not be a real sporting event, I had bought as many tickets for the “finals” as I could get my hands on. Later I sold the extra tickets as Los Angeles fell in love with the games. I made so much money that the expensive tickets I had bought for the entire family of 7 that we used ended up were effectively free since the profits covered the cost of the tickets we used. Street enterprise at its best. My tickets became worth more because the Soviets didn’t come as all Americans became Olympic fans the year we won all the golds.
Winning the race to live well with dementia is like running the 10K race at the Olympics. Everybody has to pace themselves at the beginning so that they can learn about their opponents. In the final stages of the race they speed up and sprint their fasted the last 200 meters.
A mind model of the dementia race strategy is shown below. Click the image to expand it.
I think I am winning my race to live life to its fullest while having dementia. I’m getting ready to claim that gold medal. You can win your race too. Think about what you are doing and strategize like a 10K runner. Learn all you can in the beginning and then speed up later as your new knowledge kicks in.
I Hate Political Lies and Other BS
The politicans made me do it …
Click to expand.
Sketchnotes & Dementia: A Hypothetical Example
Click on image to expand. Estimated time to develop for a NOVICE (me) = 15 minutes. The sketchnote was drawn by a person with dementia (me).
[Note. I usually write/draw note panels like this from right to left in sections because I am left-handed and it minimizes the amount of smeared ink. There is no magic in this, so use any organization that works for you.]
My Tweets on Dementia Organizations from July 19 2016
Tweets from July 19, 2016. While shortened for Twitter’s character limit, the meaning of these tweets should be fairly transparent. I believe that most of the so-called Dementia “Organizations” or “Charities” need huge restructurings of their operations in order to actually understand and attend to the needs of Persons with Dementia.
If you want to learn about non-profit organization that does its job extremely well (albeit in a different area), search information on the AIDS Healthcare Foundation in Los Angeles. Superb job. Big bang for the buck. And follow them on Twitter at @aidshealthcare.
Ever wonder what the difference is between Huba #MindModels and Buzan #MindMaps?
Ever wonder what the difference is between Mind Map techniques developed by Buzan and Mind Model theory and techniques developed by me?
Probably not.
At any rate, just in case you have an itch to figure out the difference later, here is a cheat sheet in a Mind Model. Click on the image to expand it.
Did that get rid of the itch?
Dealing with Terrorism: 5 Choices #MindModel
There are 5 basic choices, although more than 1 option could be executed simultaneously. For instance, one well-recognized American wanna-be POTUS would use options 1 and 2. One liberal blogger would combine Choice 5 (most important) with Choice 4.
Click on the image to expand it.
In the long run, Choice 5 will work best. Choice 4 eventually needs to be done no matter which other choices are made. Choices 1-3 are merely band-aids at best, and demagoguery during an election year in the worse case.
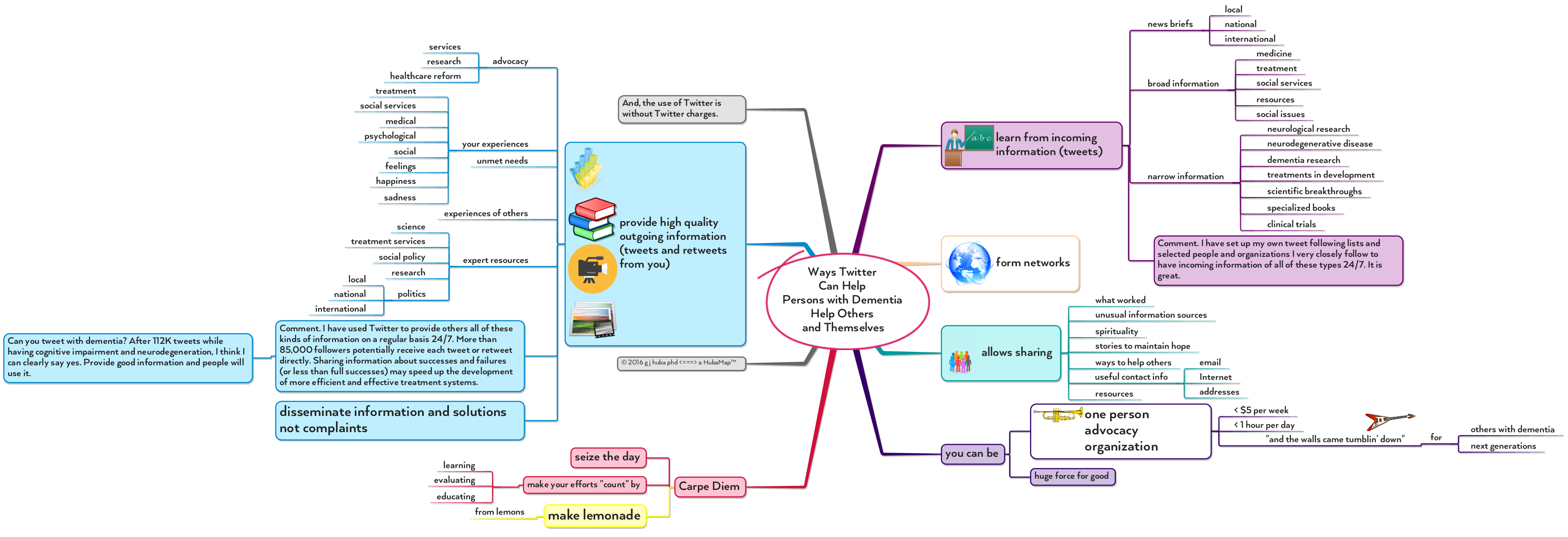
Using #Twitter for Social Good by Persons with #Dementia and Everyone Else, #MindMap
Have dementia? So do I. You and I and others can use Twitter responsibly to provide information and observations and comments to millions of others, any one of whom might use that information to make a difference in treatment systems, the development of pharmaceuticals, priorities for the use of tax dollars, or the care of a family member.
Pssstttt… these techniques are for anyone advocating for just about any social issue. Pick a good topic you know something about and become a One Person Advocacy Organization.
Click on image to expand.
Word Recognition of Dictated Notes, #Dementia, #Caregivers, Mary Poppins: #MindMap Improved #QOL
Living with dementia is all about improving quality of life (QOL). Treatments to fix up your brain are still in development. They will not happen in my lifetime. But, as I always suggest in this blog, there are some ways of using simple cognitive and behavioral methods that may make your life (and that of your family) more pleasant. When you have dementia, a better day is priceless.
There are several products on the Apple app store for iPhones and iPads that claim to promote electronic communications among patients, family members, and paid caregivers. In reviewing many, I found them — as a group — to be somewhat expensive and typically fairly difficult to use (by me, a member of the patient target group with a PhD and 25+ years of software development experience).
I have carried an iPhone and iPad with me almost continually for the past 10 years. I have always considered the voice control app Siri to be something of a “bar toy” that you can ask questions like “who won the 1923 World Series?” or “what is the dollar-euro exchange rate?” My judgment had been drawn based on the earliest versions of Siri that had significant problems in voice recognition and returned “interesting if bizarre” information in response to questions.
Then recently I watched a teen sit with her iPhone and take notes, schedule, get smart answers, and generally zip through her homework. She did not seem to be doing anything “special” to enable the phone to interpret her voice. And she got terrific and accurate translation of her spoken words into written words using Siri.
Well … I decided it was time to start acting “cool” and flexible again and seem like I was having a conversation with my friend Siri. I started to talk to Siri and “her/him/it” and tell it to take written notes. I experimented with several Apple devices and found that multiple individuals (and devices) linked on the same account can easily share notes.
Free. Nothing special required. Easy. Doing a little research, I concluded that the transcription and note taking function now work far better than ever before due to enhancements in Siri, but more importantly because of recent upgrades in the Notes app included in iOS.
There is huge potential here for Persons with Dementia to take notes for themselves easily and simply by speaking into an iPhone they carry everywhere. And for caregivers and family members to leave notes for a Person with Dementia. Or to check the PWD’s notes to see what is going on. No lost notes and I bet that many people are likely to carry their phone everywhere than to carry a pencil and notepad.
If you and Mom (or Dad or your aging friends) carry iPhones, you can easily set up a system where notes can be shared in a couple of minutes.
Comments:
1. Apple is reliably rumored to be releasing Siri for the Mac in June 2016.
2. At this time I only recommend sharing notes, not calendars. Calendars are confusing.
3. Siri also runs on the Apple Watch. Hopefully well enough to also share notes.
4. Donald Trump is reportedly suing to change the name Siri because he does not want Syrians in the US (OK, so I couldn’t resist).
The mind map below organizes the basic information about this system and provides additional details.

The slide presentation breaks the mind map into pieces. It will run automatically or you can push the pause button and then use the arrow keys to move through the presentation manually.
Siri, take a note. Get started making electronic notes with Siri many times per day.
You can change voices for Siri [male/female and in the US Version Americanish, UKish, or Australish] easily. I prefer the female British voice (the American female version is too common, the Australian female version is too upbeat and hard to follow, and I do not want a male butler or a bossy service representative voice). Mary Poppins is quite helpful, friendly, and at times scolds you. I need a nanny.
By the way, ask Siri to take a note and say this word. It will spell it correctly.
If you use Siri, you can also find out the answer to the “argument” (discussion) you having with your caregiver about how much money Lionel Messi makes in dollars, euros, pounds, or yen.
Sorry folks. I do not use PCs anymore after 30 years of frustration and bugs or Android devices so if you do not use Apple products you are going to need to explore this area on your own.
Four Types of #Apathy in #Dementia (Guide for #Family and #Caregivers) – #MindMap
Apathy is often identified as a key symptom used for diagnostic and other purposes with dementia. Apathy seems to be most often discussed for those types of dementia-causing conditions often associated with young onset.
I believe it is possible to differentiate four types of states that are identified as “apathy.” This differentiation is quite important both for the administration of drugs and behavioral exercises to fight apathy and for planning social interactions and outings for the person with dementia if you are a #caregiver or a #family member.
The following mind map shows and explains four types of apathy that I would differentiate. Click on the diagram to expand it.
Type 1 is what I would call “observer identified apathy.” Caregivers, friends, doctors, and others see an individual who does not smile or seem to react to a positive environment and assume that the person is not experiencing emotion and would like to repeat the experiences often or see the same people again. These observations may have a quite different meanings for different individuals and in fact not represent apathy. For instance, I have little control of my non-verbal expressions (face muscle control and feedback is going, going, gone) and even though I feel happy and engaged you will rarely see a smile and when I try to “force one” for the iPhones, I usually end up making a rather bizarre expression. At social gatherings I often stand by myself just watching. I am neither apathetic nor a “stalker,” rather I often disengage in large groups because I can not selectively attend to individuals or the noise is too much for me to understand what is being said. I am trying to control incoming stimuli not to ignore them. On the fringes or in a quieter space with a small group of individuals I can appear quite engaged.
Try not to over-generalize when looking at a person with dementia and assuming that they are experiencing apathy. Something quite the opposite may be happening. And I may not be ignoring you because I feel apathy or do not like you. You may simply be standing in a noisy, chaotic part of the room.
Type 2 is what I would call “true” or “experienced apathy.” The person with dementia experiences the classic symptoms.
Type 3 apathy is mislabelled depression. Many of the symptoms of depression are also indicators of apathy but the underlying causes of the behaviors may be quite different for apathy and depression. It is important to determine if the person with dementia is actually experiencing depression rather than apathy (or both) as there are medicines available that seem to be able to help control symptoms of depression.
Type 4 apathy is what I would call “deliberate apathy.” When you see me ignoring situations you find enjoyable or engaging or demanding an emotional responsible, it may be assumed that I am experiencing apathy. I might tell you that you are right, I am, but it is because I chose to for this situation. At some point as dementia progresses one may need to make decisions about which activities and people and situations are the most important and should receive as much of the rapidly dwindling supply of mental energy as possible and which should be ignored so that energy can be conserved. These are deliberate decisions that people with dementia may need to make and then adopt as part of their lifestyle. My social circle is smaller because I have had to make choices about where to direct my energy and my “ignoring” someone is not a statement of disliking or lack of concern but rather that I think my family needs my time and energy more than they do. Things I used to think were fun are ones that I may ignore or avoid now not because I fail to think that they are fun but because I have decided that other things are more fun or enjoyable for other reasons and I should invest my limited time and energy into those.
Note that several or all of these types of apathy experience may be going on in a person with dementia at the same time. It is much more complicated than it looks.

Brains are Too Precious to Destroy: #MindMap
Let’s get rid of brain destruction for recreation and entertainment once and for all.
From BIG D to little d: Your #Dementia Experience Will Differ from That of Your Grandparents and Parents
The BIG D — currently the most dreaded way to die in the world.
I occasionally get tweets when I write columns on living well with dementia stating that the writer will — if he or she gets dementia in later years — consider committing suicide. At times people imply that I should also.
I regard most of these arguments as emotional masturbation although I also know that some people will go through with such a plan. I feel very sorry for them and wish that we had a better mental health system to deal with their pain and confusion.
You saw your Mom or your Gramps suffer (or at least you thought they were suffering while they were causing work and other problems for you). It scares you, it enrages you that lifetime savings are wiped out and do not pass between generations, it messes up your own relationships with your own nuclear family. You feel powerless and guilty and angry and helpless. And very, very tired.
The BIG D your Dad and Grandmother had are becoming the little d. Treatments are being developed for all types of dementia causing conditions, and you can expect them to be available in the not too distant future of 10-20 years. Behavioral interventions can greatly improve quality of life. Treatment will get less expensive over time (and even less so if we nationalize Big Pharma for the good of the world). Improved housing, professional caregiving, education of healthcare providers to make early identifications of impending dementia, and cost saving measures make it easier and cheaper to have a continuing good quality of life while living with dementia. Yes, I am too advanced to probably benefit much from forthcoming huge changes in dementia care and treatment, but my children and yours will which is something to look forward to.
OK, you are sitting there saying this guy is full of shit. Not really. In 1992 I started two decades of evaluating and helping improve some of the most creative and innovative programs for HIV/AIDS treatment and prevention funded by the US government. From 1992-6, I watched literally dozens of my friends and coworkers die of AIDS 20 to 40 years before their life expectancy in an AIDS-free world. In the mid-90s I had dozens of additional friends in their 20s through 40s with HIV/AIDS who had a life expectancy of a few years and a miserable death ahead of them. Then came the medical miracle of antiretroviral drugs. Almost all of the folks I was close to who moved onto the new treatment regimen are alive now 20 years later and living pretty “normal” lives. Many moved from being uneducated street youth to PhDs and program administrators and federal employees and teachers and parents. Yes, parents. And quite good ones. Also, good taxpayers.
The BIG H (HIV/AIDS) was tamed for those who could be identified early and were in countries where antiretroviral drugs could be made available for a reasonable cost within differing levels of national average income. Much more remains to be done to fully tame HIV/AIDS, especially in Africa, a continent ignored by the rich nations. But the tools are there and the money should be. Should the big governments of the world not be willing to make this happen, perhaps the big religions of the world who have amassed reserved of valuable property and cash could use their funds to solve these medical problems.
I have no doubt the BIG D can be tamed like the BIG H and that the same problems with sharing the costs for treatment in the developed and undeveloped world will occur. And I greatly doubt various political factions will want to spend the dollars needed for research and developing treatments and making them universally available along with lifestyle training programs to help prevent certain kinds of dementia.
Stop thinking about suicide if you get dementia and start thinking about electing politicians who know that the horrible diseases of the past and their somewhat milder versions of the present can be tamed far more rapidly if resources are turned into medical research and treatment rather than bombs and trying to control countries with different religions and peoples of different colors than your own. Elect someone who has the guts to take on the aggressive capitalists of Big Pharma and conservative governments.
And do not send me tweets suggesting that you are morally superior to me because you will commit suicide to save society money if you get dementia. I think that is VERY wrong.
The BIG D is going to be a disease that will be solved eventually. And you will have a milder and less lifestyle disrupting version than your grandparents and parents. Speed up the process of making these advancements by fighting to devote resources to the development of the solutions. Emotional masturbation that maybe you will commit suicide in the future to “save society the cost after it is helpless for me” is not doing a damn thing to solve the mysteries of the neurological diseases that cause dementia. Devote the later stages of your life to looking for solutions, not giving in and accepting misery for yourself and your descendents or thinking Donald Trump is going to solve your problems.
Dementia care and treatment is changing for the better in a manner that is far more rapid than the garbage you read about in the news channels on the Internet. On the other hand, the politicians who allocate public monies are being more stoopid about health issues than ever, a fact rarely stated in its full ugliness in the press.
Here is how I see the situation. Click on the mind map to expand it for easier viewing.
And don’t give up. It is not going to be as bad as it was for your grandparents and parents. And you have lots of technologies and treatment innovations to make your quality of life better.
And use the time you gain from the advances in dementia treatment and care to help speed the progression of the work to solve this and all other diseases.
Enhanced Suggestions for #MindMaps Specifically Designed for #Twitter