While having dementia, I realized that I could not always depend on myself to be able to remember what had happened to me over time. Symptoms? Mood? Problems? Successes?
One of the most effective ways to improve medical treatment is for the healthcare provider(s) and the patient to work as a team. Notice that one of the first things your doctor asks is “how are you?”
How you answer that question will greatly determine how much you and healthcare providers can accomplish during the appointment.
When friends ask you how are the automatic response is “fine” for most people. Same thing for when doctors ask that at the beginning of an appointment.
Let’s be real here. When you have dementia, things are not going to be fine ever again. By just replying “fine” your friend or healthcare provider might infer that you are avoiding answering honestly or even worse, they will believe that you are “fine.”.
About a year after my diagnosis 10 years ago, I stopped just answering “fine” and adopted the following response.
“For someone who has dementia, II am doing as well as anyone can realistically expect, and many times even better than that. I am eternally grateful to my doctors, family, and friends.” Or something more informal but expressing the same thoughts
Now, if you want to get the most out of your doctor’s appointment, you need to quickly, fully, and accurately tell your doctor what “fine” or “terrible” means to you..
Doctors are scientists trying to use all of their skills to determine what they can do to make your life better and more comfortable.
They need DATA. Not just data that comes back from a blood test or your blood pressure or weight but data on how your medications are working, how you get through your day with dementia, events that may have happened like a fall, and side effects you get from your medications.
I know how to deal with the need of the doctor for DATA to fine-tune your treatment. You figure out what she needs to know and you start to document what is going on.
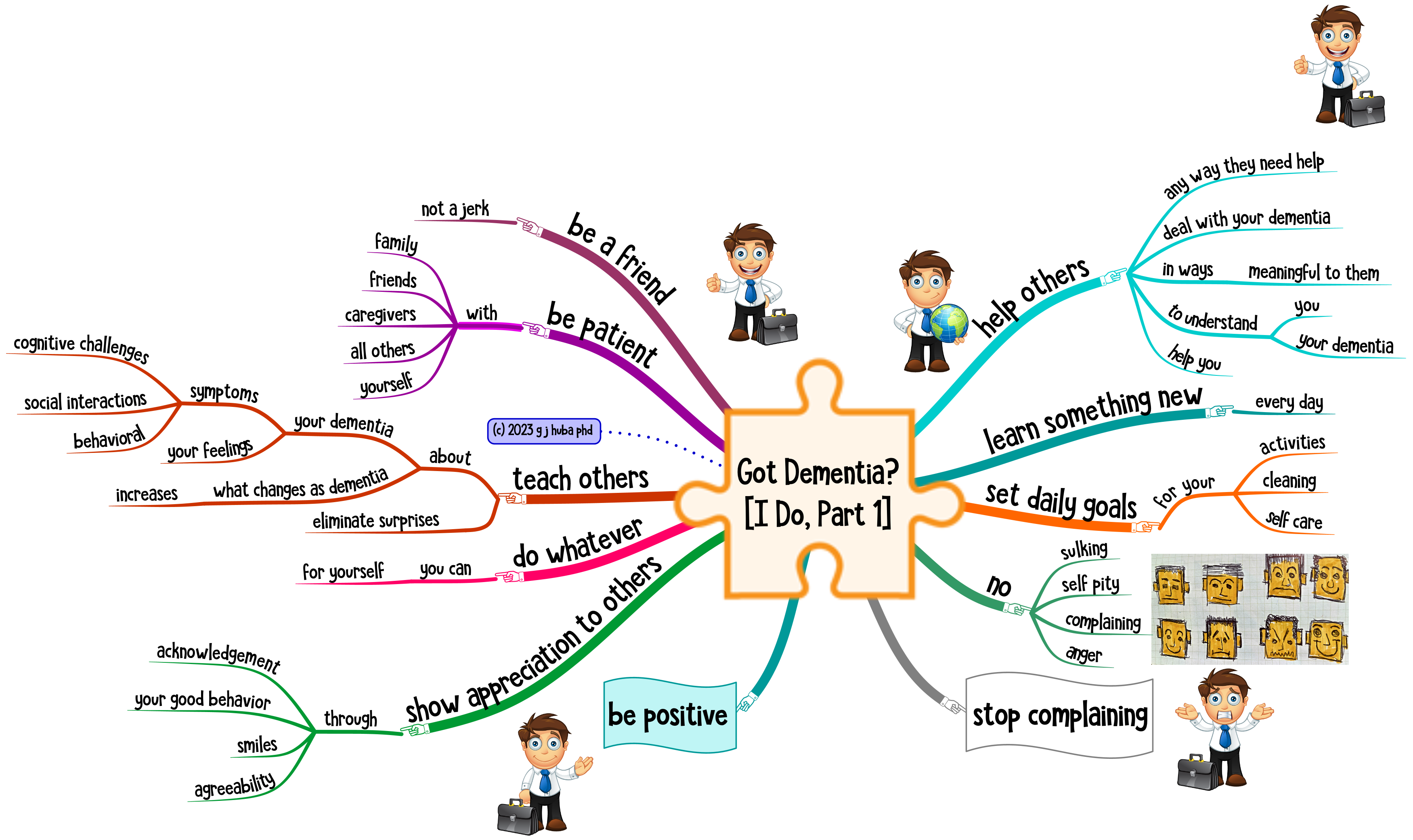
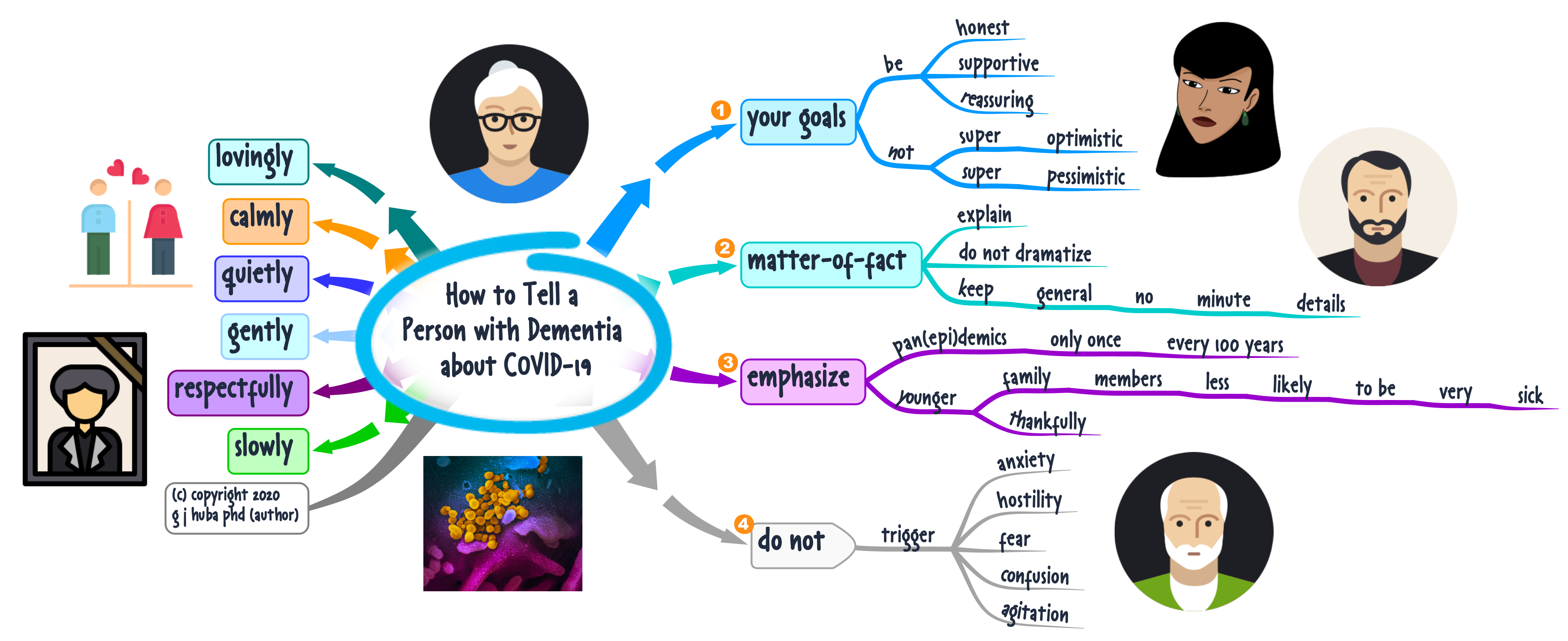
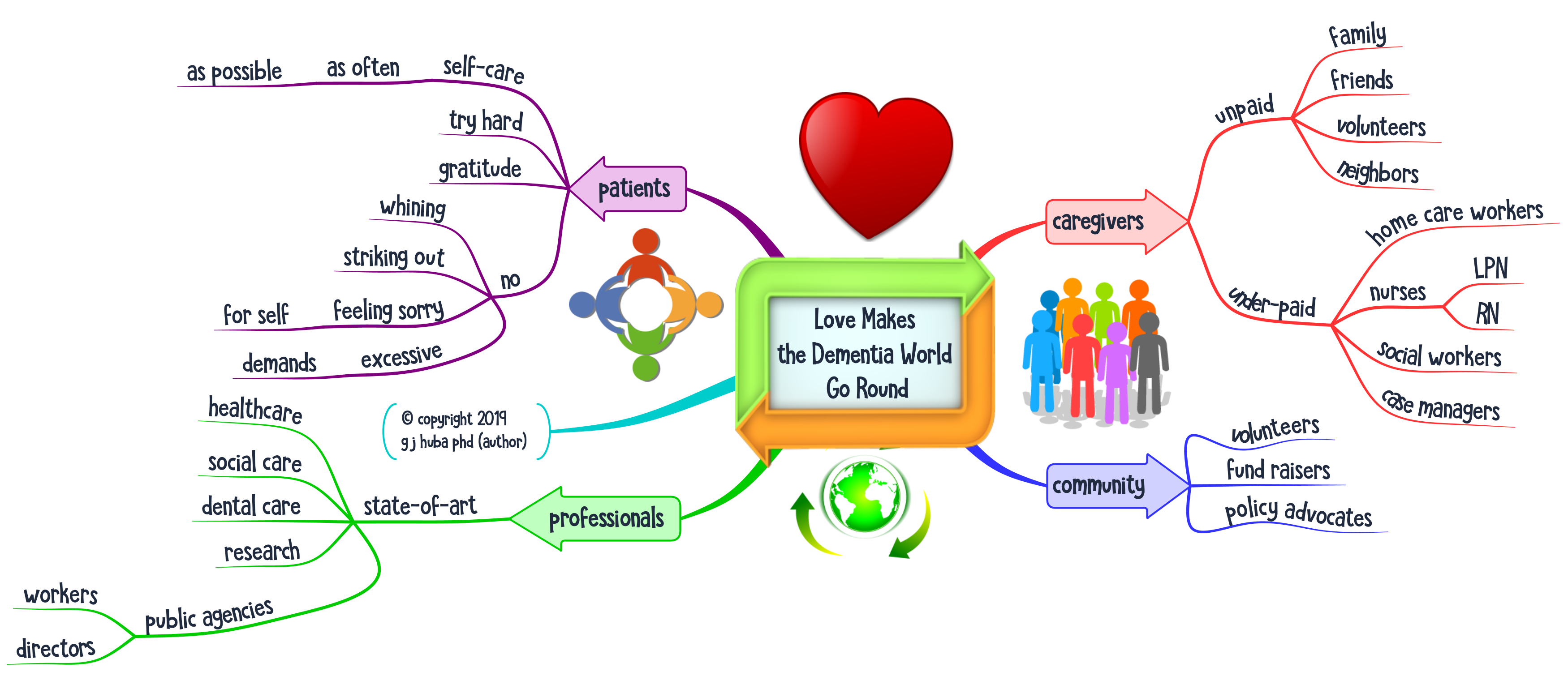
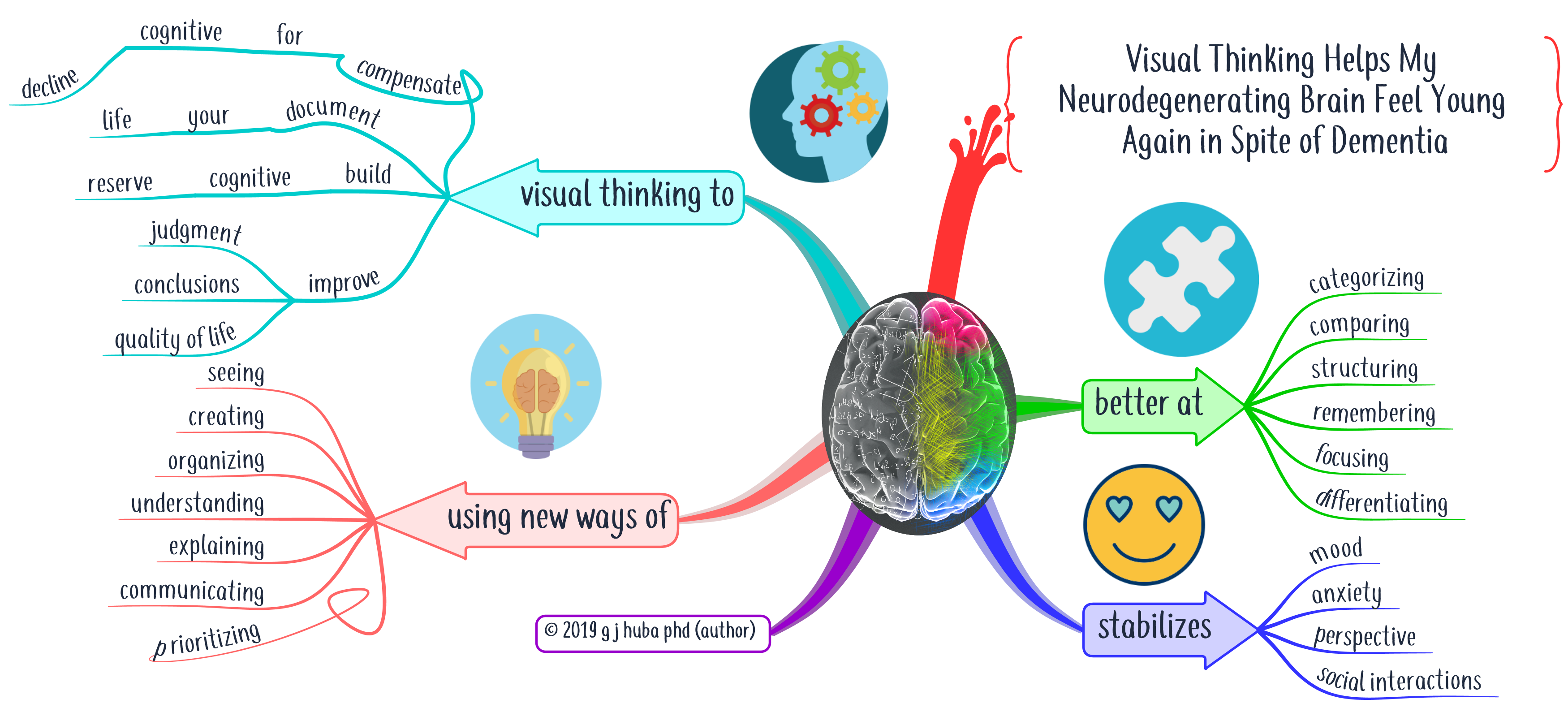
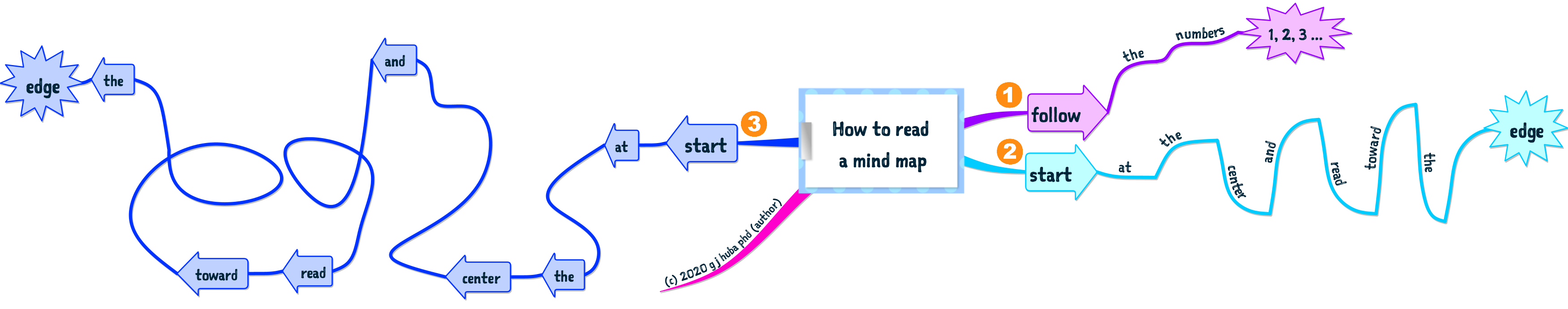
So I started to prepare for the appointments by spending a few minutes developing a mind map that would help me remember what to say in my appointment using the mind mapping techniques I talk about in this blog. This helps me capture in more detail how the 3 or 6 months between appointments had been going. And it helped me understand how the things I did and the environments I faced determined the outcomes of my treatment.
II started collecting some data about myself and I brought some mind maps to my doctor appointments regularly. It got much easier for me to explain how I had been doing since my last appointment. How well did my medications work? Did they have side effects? How did I structure my day and how did I get along.
Several doctors saw me consulting a bright and clear mind map on my lap. In several cases, they (my neurologist and my internist) almost grabbed the display from my hands. I now have dozens of mind maps scanned into my medical chart.
The mind map below shows some of the data I collect and how I present it to my doctors.
Expand the image by clicking on it.

I’ll be creating many more blog posts on how to work with your healthcare provider and provide her with data that helps her understand what works well for you. Watch this space.
Like this:
Like Loading...