Last week (June 14, 2017) I received an email from a close friend with a link to an article generated by the North Carolina station of the National Public Radio a month ago. Along with noting that the research process was not what it once was — specifically that I had received a description of a study carried out in India from a psychologist in Israel with a summary of a radio broadcast generated about five miles from my home.
The changes in how we think, process and access information, and communicate change dramatically annually (as well as monthly, weekly, daily even). But is everyone changing how they fit to match our modern world and its information use possibilities?
People of many different income, education, social, and other strata within Indian society took EEGs to study their alpha brain patterns. There were many differences between the way that their brains seemed to work as measured by EEG indicators that could potentially be explained by differences in exposure to different levels and kinds of technologies.
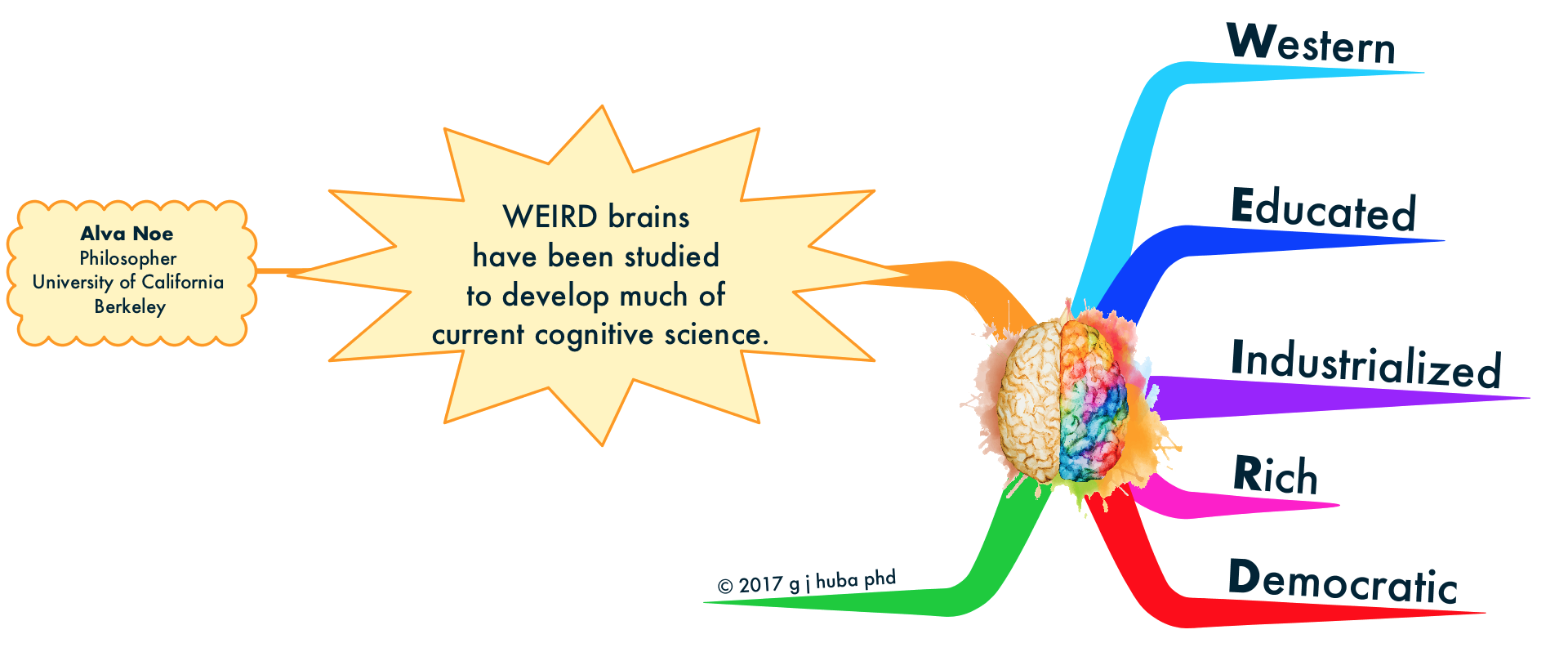
A summary of the work appears here and was written by the University of California, Berkeley, philosopher Alva Noe. Noe discusses how brain wave patterns may have changed as individuals are exposed to the dramatic new information access and processing annually. The original scientific research by and appears here. Noe notes that one of the “problems” in our current conceptions of neurocognitive science is that virtually all of the experimental results have been derived from “WEIRD” brains, that is individuals educated in current technologies within western, industrialized, rich democracies. The Indian results suggest that there are different patterns of “NORMAL” brain waves among individual from other backgrounds.
I find Noe’s ideas to be quite compelling.
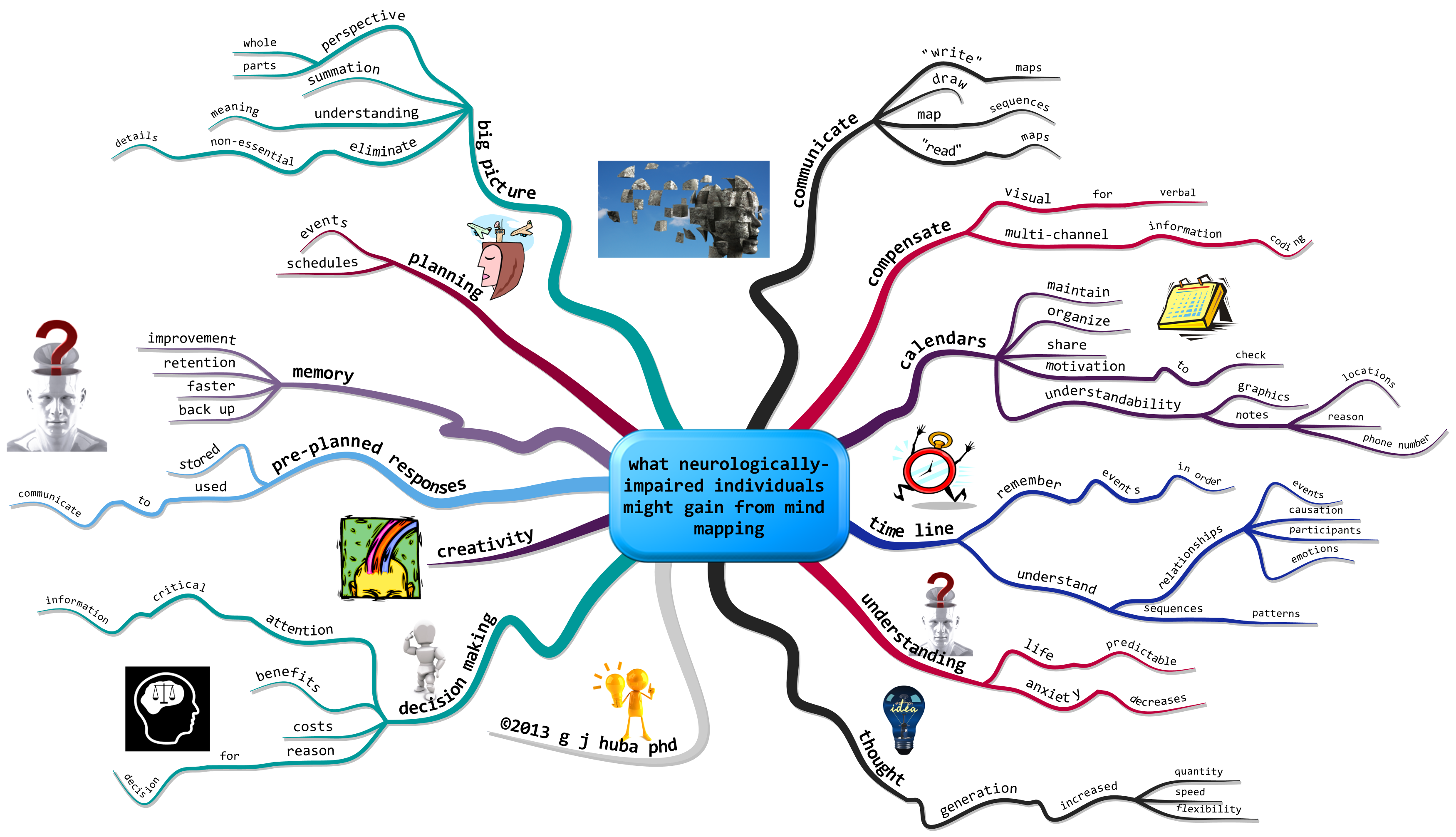
Click to open the mind model (aka mind map).